Archives of Preventive Medicine
The effectiveness of interventions for improving the uptake of Intermittent Preventive Treatment (IPT) for malaria control among pregnant women in sub-saharan Africa: A systematic literature review
Chukwuma Ernest Egbujor1, David Chinaecherem Innocent2*, Uchechukwu Madukaku Chukwuocha2, Uzochukwu Godswill Ekeleme2, John Chigozie Ekenze3, Ugonma Winnie Dozie2, Chiagoziem Ogazirilem Emerole2, Igiri Vivian Chika2, Nanush Damarlapally4, Ihuoma Chimdimma Dike2 and Stanley Chinedu Eneh5,6
Cite this as
Egbujor CE, Innocent DC, Chukwuocha UM, Ekeleme UG, Ekenze JC, et al. (2023) The effectiveness of interventions for improving the uptake of Intermittent Preventive Treatment (IPT) for malaria control among pregnant women in sub-saharan Africa: A systematic literature review Arch Prev Med 8(1): 008-019. DOI: 10.17352/apm.000032Copyright
© 2023 Egbujor CE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: Malaria in pregnancy is a public health problem in Sub-Saharan Africa (SSA) that continues to account for increased morbidity and mortality among women. Anemia, maternal death, stillbirth, and low birth weight are complications associated with malaria in pregnancy. Adoption of recommended malaria control measures such as intermittent preventive treatment (IPT) remains a problem among pregnant women in SSA.
Aim: We aimed to evaluate the effectiveness of interventions for improving the uptake of IPT for malaria control among pregnant women in SSA.
Methods: The MEDLINE, Pub-Med CINAHL, and African Journal Online databases were subjected to a systematic search for Randomized Control Trials (RCTs) for the review. The studies were screened for eligibility and evaluated for methodological quality using the Cochrane Risk of Bias Tool. The screening process was carried out by one reviewer to help reduce the amount of time and resources that would have been used by two reviewers. The narrative synthesis approach was adopted for data analysis and synthesis after extraction from selected studies.
Results: A total of 1679 articles were found, and the comprehensive screening of the search results left a total of four RCT studies that were deemed eligible for inclusion in the review. All the included studies adopted two-arm comparisons, i.e., the control and intervention groups. The findings revealed that three studies evidently reported increased uptake of intermittent preventive treatment in pregnancy using sulfadoxine-pyrimethamine (IPTp-Sp) doses among pregnant women following community-based promotional activities.
Conclusion: Our review revealed the effectiveness of community-based promotional activities as effective interventions for improving uptake and possibly compliance to intermittent preventive treatment in pregnancy (IPTp) and antenatal attendance. This evidence and findings will guide policy-makers and health agencies in the SSA region to plan further interventions.
Abbreviations
ANC: Antenatal Care; IMB: Information Motivation and Behavioral Skills; IPT: Intermittent Preventive Treatment; IPTp: Intermittent Preventive Treatment in Pregnancy; PRISMA: Preferred Reporting Item for Systematic Review and Meta-Analysis; RCT: Randomized Control Trials; SP: Sulfadoxine-pyrimethamine; SSA: Sub Saharan Africa; WHO: World Health Organization
Introduction
Malaria constitutes a global burden and has posed detrimental concerns among various groups of the population [1]. Malaria in pregnancy (MIP) contributes to devastating maternal and neonatal outcomes, including maternal anemia, maternal death, stillbirth, spontaneous abortion, and low birth weight. In 2020, around 11.6 million African women were infected with malaria during their gestation period, resulting in 819,000 low-birth-weight newborns [1]. In order to mitigate the consequences of malaria in pregnancy in moderate to high malaria transmission areas, the World Health Organization (WHO) recommends that pregnant women receive Intermittent Preventive Treatment during pregnancy (IPTp) with sulfadoxine-pyrimethamine (SP) [2-7]. IPTp was found to decrease the incidence of low birth weight by 29%, severe maternal anemia by 38%, and neonatal mortality by 31% [8]. IPTp is also one of the few malaria prevention interventions with peer-reviewed evidence confirming its effectiveness in lowering infant mortality, resulting in a significant reduction in malaria-related deaths [9]. Further, although there is increasing parasite resistance to SP in some areas, IPTp remains a highly cost-effective, lifesaving strategy to mitigate the adverse effects of MIP in pregnant women in SSA [8,10-12]. The WHO’s (2014) policy encourages the use of IPTp-SP in areas with moderate to high malaria transmission, starting as early as the second trimester and continuing every scheduled antenatal care (ANC) visit thereafter, at least one month apart, until delivery [13].
Understanding the etiology behind increasing malaria incidence during pregnancy is imperative. However, several reports have focused on community promotion activities on various contemporary issues in the community. Notably, it is pertinent to explore the efficiency of these attempts in improving malaria control strategies in the community [10,12,14]. Pregnant women are one of the high-risk groups, with several publications reporting rising statistics in maternal mortality. The uptake of intermittent preventive treatment in pregnancy has been suggested by several reports, but evidence of the effectiveness of community health promotional activities on the uptake of intermittent preventive treatment in pregnancy remains scarce. However, pregnant women in SSA are faced with numerous challenges with a significant paucity of data. However, it is due to the magnitude of this problem that our review aims to explore community promotion activities and the effectiveness of interventions for improving the uptake of IPT for malaria control among pregnant women in SSA.
Methodology
A thorough search of the literature was carried out in MEDLINE, CINAHL, and African Journals Online databases. The PICO framework was used to define inclusion and exclusion criteria for studies included in our study.
Inclusion criteria
Types of studies included: This study relied on information gathered from peer-reviewed journals to review the effectiveness of interventions for improving the uptake of intermittent preventive treatment (IPT) for the control of malaria among pregnant women in SSA. The study included randomized control trials. Non-randomized controlled trials were not considered eligible for inclusion.
Participants: Only pregnant women from SSA are eligible.
Types of intervention: Interventions in this systematic review include those for improving the uptake of IPT and compliance with sulfadoxine-pyrimethamine. This is the drug recommended by the WHO for IPT during pregnancy for the control of malaria.
Types of outcome: The primary outcome of interest in the included studies was an uptake and compliance/non-compliance with IPT for malaria control among pregnant women.
Exclusion criteria
Studies were excluded from this review if they were conducted in regions outside sub-Saharan Africa, and focused on non-pregnant women, nursing mothers, or pregnant women living with HIV/AIDS. Also excluded were interventions that focused on drugs not recommended by WHO for IPT, such as studies focusing on the use of dihydroartemisinin-piperaquine for IPT or the cost of the interventions. Finally, qualitative studies, commentaries, literature reviews, non-randomized trials, cohort studies, non-controlled pre and post-studies, observational studies, editorials, and letters were also excluded (Table 1).
Identification of eligible studies
Electronic resource
The following electronic databases were searched:
- MEDLINE
- CINAHL
- African Journals Online
All resulting articles were screened, and eligible articles were included in the review. Keywords and MeSH terms were developed by using the PICO framework (Population, Intervention, Comparison/Context, and Outcome) [17]. The search process was repeated at the end of the review to identify recent studies published in the last few weeks.
Search strategy
The search of electronic databases mentioned above was developed using suitable combinations of keywords, which was guided by the PICO framework, and each PICO element formed one search domain. Search terms were used with appropriate Boolean operators.
Search terms related to the population search domain are as follows
“Pregnant girl*’’ OR ‘‘pregnancy N2 girls’’ OR ‘‘pregnancy N2 young adult’’ OR “pregnant wom?n” OR pregnancy N2 Sub-Saharan Afri*”
Search terms used for the intervention search domain are as follows
“Intervention*” OR “training*” OR ‘‘educat*’’ OR “teaching*” OR “program*” OR “initiative*” OR “stateg*” OR “seminar*” OR “campaign*”
Search terms used for context search domain are as follows
“Malaria N3 prevention*” OR “Malaria N3 control” OR “Jungle fever N3 prevention*”OR “Jungle fever N3 control’’ OR “Plasmodium falciparum*” OR “drug*” OR ‘‘antimalaria*” OR “anti-malaria*” OR “intermittent preventive drug*” OR “intermittent preventive treatment” OR ‘‘IPT’’ OR “sulfadoxine- pyrimethamine*” OR “anti-Plasmodium falciparum*”
Search terms used for outcome measures search domain are as follows
‘‘Change in behaviour’’ OR ‘‘altered behaviour’’ OR ‘‘modified behaviour’’ OR “complian*” OR “uptak*” OR “accept*” OR “adheren*” OR “Adherence to sulfadoxine-pyrimethamine” OR “Antimalarials* N5 Administration’’) OR (“Antimalarial N5 dos*”) OR (“Antimalarials* N5 dos*’’) OR (“Antimalarial* N5 dos*’’) OR “Drug* N5 administration schedule” OR “Drug combination*’’ OR “self-care” OR “self-monitoring” OR “self-medication’’
The above search was conducted on the MEDLINE and CINAHL databases. The African Journal online database was searched using the keyword (“Intermittent Preventive Treatment”) because Boolean operators and comprehensive systematic searches are not supported on the database.
Data collection and analysis
Selection of studies: Search MEDLINE, CINAHL, and African Journals online. Online databases were conducted on the 19th of November, 2021, and search results from each database were documented. Search results were transferred to electronic reference management software (RefWorks). Duplicate articles within and between the databases were identified and removed. Further screening of the titles and abstracts was carried out. The full text was evaluated thoroughly against the inclusion and exclusion criteria for the final selection of the articles.
Data extraction: Data extraction was achieved through the reading of the studies included in the review and extracting data or information relevant to the question of interest. Information contained in the electronic tool (Excel spreadsheet) created for this review included the name of author and year of publication; study groups (inclusion and exclusion criteria); participant’s characteristics (age, ethnicity, and educational level; socio-economic status); interventions; control and outcomes of significance to the review question and specific objectives.
Quality assessment: The methodological quality of the included studies for this study was assessed using the Cochrane Collaboration’s Risk of Bias (RoB) Tool [18]. The Cochrane risk of bias (RoB) tool involves the assessment of the risk of bias arising from each of six domains (generation of the allocation sequence, concealment of the allocation sequence, blinding, incomplete outcome data, selective outcome reporting, and other biases).
Included studies were assessed against the six domains of the tool, and if the first three questions were answered with a YES with no vital concerns relating to the last three domains, the study was classified as having a low risk of bias [18]. Studies assessed as having two or more domains answered with UNCLEAR or NO were classified as having an unclear risk of bias, whereas studies with three or more domains answered with UNCLEAR or NO are assigned a high risk of bias [18]. These steps are important in order to minimize bias in the conclusions of a systematic review and to consider the potential limitations of each eligible study [18].
Results
Search results
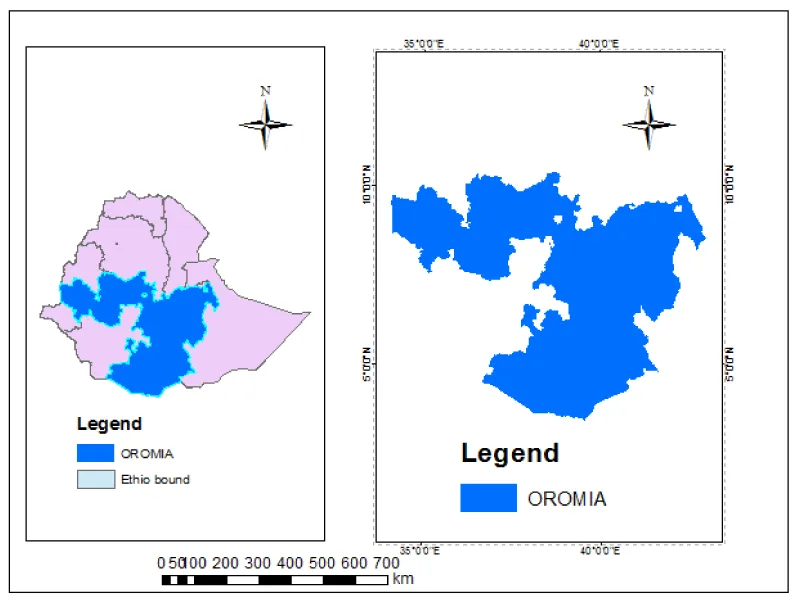
Considering the search results of this study from a combination of multiple databases, MEDLINE produced the highest number of articles (n = 1208) during the search, followed by CINAHL and African Journal Online (n = 295 and n = 176 records, respectively). A total of 1679 articles were found and 14 articles were excluded as duplicates. The titles and abstracts of the remaining 1665 articles were screened thoroughly, and a total of 1653 articles were excluded as not meeting the selection criteria and relevance of the study. The 12 resulting articles were further assessed for eligibility. One of the studies was a replica of an included study; hence, it was excluded. Four studies were found to have provided incomplete details on the required RCT design for the comparison of intervention and control groups for IPT malaria intervention, while three studies utilized a research perspective differing from the quantitative design. As a result, a total of eight publications were excluded from the study based on eligibility assessment for study design. The comprehensive screening of the studies left a total of four studies that were deemed suitable for inclusion in the review [20-23]. All of these studies were published in English in peer-reviewed journals. A detailed study selection process is shown in Figure 1. Adapted from The PRISMA Group (2009).
Description and characteristics of the included studies
From these studies, it was revealed that the randomized clinical model was adopted; one of these studies was conducted in a single health center [22], while three other studies were carried out in multiple health centers [20,21,23]. Of the four studies, two were carried out in Burkina Faso [20,23], one in Karagwe, Tanzania [21], and the other was executed in Maiduguri, Northern Nigeria [22]. Table 2 below shows details of the study population and sample sizes of the selected trials.
The types and design of the included studies
All the suitable studies had two-arm comparisons, i.e., the control and intervention groups [20,21-23]. The objective of one of the studies was to determine the impact of the community approach on increasing the uptake of 3 or more doses of IPTp [21]. Another article compared the effects of community-based interventions on the level of uptake of IPTp [23]. Balami, et al. assessed the effect of health educational interventions based on information–motivation–behavioral skills (IMB) on the uptake of IPTp among pregnant women [22]. The other study assessed the delivery of IPTp by community health workers to inform the level of IPTp uptake and ANC visits [20].
The two cluster randomized trials, Gutman, et al. [20] and Gies, et al. [23], were conducted over a period of two years and 15 months, respectively. Kinyina, et al. conducted their study within the span of a year [21], while Balami, et al. conducted it in less than six months because of the participant’s availability and the nature of the study objective [22]. Two of the included trials recruited participants for the study with a designated sample size determinant at a 5% confidence interval with the sample formulae of RCT with continuous outcomes [22,23]. All studies compared ANC visits among the intervention and control groups [20,21-23]. However, only three studies evaluated the effect of ANC on the uptake of IPT (sulfadoxine-pyrimethamine) [20,21,23]. The study by Balami, et al. [22] failed to give an account of the effect of ANC on the uptake of IPT. Table 3 below illustrates the study objectives of the included studies and the description of their methods and RCT design.
The characteristics of the participants in the included studies
A total of 3988 women participated in the included studies [20,21-23]. The study by Balami, et al. [22] noted that the socio-demographic age characteristics of the included women in the intervention group were between 15 and 40 years old and 17–45 years old in the control group. Another study included women aged 15–49 years of age in both groups [21]. Furthermore, Gutman, et al. [20] and Gies, et al. [23] reported the ages of the included women in both groups as between 18–49 and 14–41 years, respectively. However, Gutman, et al. [20] failed to record the women’s mean age standard deviation (SD). Balami, et al. [22] found the mean age (SD) of women to be 26.1 years (± 5.8) in the intervention group and 26.9 years (± 5.9) in the control group of the study. Also, Kinyina, et al. [21] and Gies, et al. [23] recorded the women’s mean+SD as 34.5 ± 1.204 and 31.2 + 4.1 in both intervention groups, respectivel±y, and 38.9 ± 3.457 and 33.7 ± 2.6 in the control groups, in the same order.
All the studies acknowledged informed consent for ethical consideration for the participants recruited [20,21-23]. Two studies did not report details on the ethnicity of participants, possibly because of the focus adopted [20,21]. Table 4 below depicts the summary of the baseline characteristics and demographic data of the study participants in the respective studies.
Intervention
Based on our analysis, it was observed that the studies focused on peripheral healthcare settings and strategically assigned community promotions to their intervention arm.
Two out of four included studies introduced training workshops for healthcare providers from participating health centers, which were delivered by one of the investigators and included an update on malaria prevention in pregnancy, the rationale for IPTp-SP, and practical sessions for data collection (collection of biological samples and administration of study questionnaires) [20,23]. Two of the studies had ANC providers advised to give two doses of SP at the beginning of both the second and third trimesters of pregnancy during the intervention period [21,23]. In the studies by Gutman, et al. [20], Kinyina, et al., [21], and Gies, et al., [23], IPTp-SP was administered through directly observed therapy (DOT) to the intervention (community promotion group) and control group. One study implemented DOT by providing a plastic jug and goblet at each health center for drinking water in order to supervise SP intake [23]. Furthermore, Gutman, et al. [20] ensured the first dose of IPTp-SP was always given as DOT at the health facility to ensure that a health provider confirmed the woman’s gestational age and initiated IPTp after the end of the first trimester.
In two of the studies, SP tablets were provided at the health centres for all pregnant women attending ANC in preparation for the promotional and delivery campaign in the intervention area [20,23]. In the study by Balami, et al. [22], the intervention group received health education on malaria for 4 hours, strictly guided by a module developed by the researchers based on the information-motivation-behavioural skills (IMB) model. Preventive measures, complications of malaria during pregnancy, and clinical features of malaria were the four sections of the module delivered to participants in the study by Balami, et al. [22]. Table 5 below summarizes the differences in the intervention and control groups of the included studies.
Enrolment and follow-up
All the included studies reported that participants were enrolled following their informed consent for inclusion in the study [20,21-23]. Some of the study subjects dropped out due to death or removal from analysis. Furthermore, based on the follow-up of participants, one study noted that those enrolled in the study were informed about the dangers of malaria for pregnant women and their babies and early and regular ANC attendance was promoted to ensure timely IPTp-SP uptake during follow-up [22]. This helped in the follow-up of participants in the study.
Outcomes and results of the included studies
Considering the outcomes of the interventions in the included studies, one of the studies revealed primary outcomes such as placental parasitemia, anemia, and birth weight [23]. Also, secondary outcomes were measured based on ANC visits and the total number of doses of IPTp-Sp [23].
Three of the studies reported participants’ uptake of SP as an IPTp [20,21,23] except Balami, et al. [22] which did not report. The uptake of IPTp using coverage parameters was reflected by Gutman, et al. [20]. The number of ANC visits was reported in 3 studies [20,21]. However, it was not reported in the study by Balami, et al. [22] Only Gies, et al. [23] compared the timing of the ANC among participants visiting the facility, while two other studies only provided information on the visit [20,21].
Reports from three studies showed increased uptake of IPTp-Sp doses among pregnant women recruited for the study following promotional activity [20,21,23]. Complete uptake of IPTp-SP was recorded as 71.8% with and 49.1% without promotion (P = 0.008) in the study by Gies, et al. [23]. [20] found that by the endline, IPTp administration was higher in the intervention than in the control, with a DiD of 17.6% for IPTp3 (95% CI 16.3, 51.5; p-value 0.31) and 20.0% for IPTp4 (95% CI 7.2, 47.3; p-value = 0.15). A difference in differences (DiD) analysis was conducted to assess the change in coverage of IPTp and ANC over time.
Furthermore, Kinyina, et al. [21] revealed that of the pregnant women in the intervention group, 98.5% received IPTp3+ compared to 55.7% in the control group. The study by Balami, et al. [22] showed, based on the outcomes of the intervention, that the participants’ knowledge of IPTp measures at baseline ranged from 4.4% to 93.3% with a mean (SD) of 60.0 (15.8) percent. Their total motivation scores ranged from 44.4 to 100± with a mean (SD) percentage score of 81.6 (10.8) percent, while total behavioral skills scores ranged from 42.9 ± to 100%, with a mean (SD) percentage score of 83.7 (12.7) percent. At baseline, there were no significant differences in the mean knowledge (p = 0.216), motivation (p = 1.000), and behavioral skills (p = 0.651) scores of the groups at baseline [22]. However, the degree of easing or taking all IPTp medicines was reported higher among the intervention group at 4 months post-intervention after questionnaires had been scored on the Likert scale, indicating the effectiveness.
According to the study by Gies, et al. [23], women who had attended antenatal at least once during pregnancy were followed up based on the enrolment criteria of the study. Almost all women in the study area who had been followed up until delivery attended an ANC at least once during pregnancy (96%, 2,154 of 2,240). In one of the four studies [20,21,23], half of those who attended ANC completed the national standard of three or more visits (53%, 1,142 of 2,154), and 20% (434 of 2,154) attained the WHO standard of four or more visits in three studies [20,21,23].
The study by Kinyina, et al. [21] revealed that, based on the relation between ANC attendance and SP uptake, the number of SP doses a woman had received throughout pregnancy was strongly related to the number of ANC visits completed by the time of delivery. The coverage with two or more doses of SP was 46% with two ANC visits and increased to 83% after three visits, and to 97% after four or more visits (p = 0.009) [23]. Gutman, et al. [20] demonstrated that altogether 374 and 360 women were included in the baseline and endline surveys, respectively. At baseline, women received a median of 2.1 doses; by end line, women received a median of 1.8 doses in the control group and 2.8 doses in the intervention group (p 0.0001).
Bias in assessment in included studies
The findings of the quality assessment of the included studies using the Cochrane Effective Practice and Organization of Care (EPOC) risk of bias tool are reported below (EPOC, 2017).
Selection bias: The studies included in this review randomized participants into one intervention and one control group [20,21-23]. Furthermore, based on the selection of health facilities among the included studies, three of the studies were conducted in multi-centres to adjust for random sequence generation and selection bias [20,21,23], while one was conducted in a single-centre [22].
Allocation, concealment and detection bias: The decision of allocation concealment in three of the four included studies is not clear, albeit the predisposition in RCTs was not grounded [20,21,23]. According to Maher, et al. [24], a randomized control trial is necessary to be subjected to allocation concealment. Nevertheless, evaluating the outcomes by blinded assessors and acting on them prevents detection bias [25,26]. Three of the four studies did not exhibit participant blinding because they did not report it [20,21,23]. This study examined the detection bias standards from studies that randomly assigned participants to one of two groups (one intervention and one control group) [20,21-23]. One of the studies stated that the community educators were informed about the community health promotion of IPTp-SP and the objectives of the study [23].
Blinding of participants and personnel (performance bias): Three of the four participants in these studies were not blinded or did not report procedures for blinding the participants in the study following promotion or health education on IPTp uptake among pregnant women [20,21,23]. However, the study by Balami, et al. [22] reported that the study was double-blinded; in the study, participants, as well as the enumerators, were blinded to the groups they belonged to, as it was not disclosed to them, and it was not indicated on their study cards. The enumerators were also not involved in any other part of the study [22].
Attrition bias: Attrition may occur due to dropout, withdrawal, incomplete information, inappropriate exclusion, or death of participants [21]. did not report attrition bias. However, Gutman, et al. [20], Balami, et al. [22], and Gies, et al. [23] discussed attrition bias in their respective studies. In the study by Gies, et al. [23], a total of 2,766 pregnant women registered for the study, but 208 (7.5%) were lost during the follow-up because 8 (0.2%) withdrew consent, 262 (9.4%) gave birth before the commencement date and were a priori excluded, 45 (1.6%) were lost due to miscarriage, and 3 (0.1%) died due to premature childbirth. This left 2,240 deliveries for the analysis. Study from Balami, et al., [22]: at the end of the study for the intervention group, 25.3% dropped out, as against 31.2% dropped out for the control group. In the study by Gutman, et al. [20], for the control group, baseline participants were 188, while for the end line, the participants were 180. For the intervention group, the baseline participants were 186, which dropped to 180 participants at the endline. Reasons for dropout were not reported in the studies [20,22].
Reporting bias: Based on the objectives of the study, it was reported in three of the four studies that age, ethnicity, religion, gravity, level of education, number of ANC visits, and uptake of IPTp-SP were concerned baseline characteristics of participants in the study [20,21,23]. However, Balami, et al. [22] reported the knowledge outcomes of participants as well as baseline characteristics of women in the RCT study.
Other bias: The included studies could have been subjected to any of these biases, thus it is imperative to report them. However, this was not accounted for in the included studies; hence, it was marked as unclear. Table 6 below explains the Cochrane tool adopted to assess the RoB in each of the included studies.
Included studies funding
Only two of the studies reported an external funding source [20,23]. The two other studies reported that the studies were not funded externally [21,22]. It is unclear if these allocated funds have impeded community promotion among participants, as limited research funds could most likely reduce the quality of the study. However, the studies by Gutman, et al. [20] and Gies, et al. [23] clearly explained that their studies were funded by generous support from the United States Agency for International Development (USAID) and European Union INCO-DEV programme with strategic consistency and adherence to the framework of an agreement to avert bias.
Narrative synthesis of results from studies
All studies have considerably large samples, and the minimum sample size among the studies was 372 [22], and the maximum sample of participants recruited in one of the studies was 2240 [23]. Considering the impact of community-based promotion on the uptake of IPTp, Gies, et al. [23] noted the significant effect of the promotion on the uptake of intermittent preventive treatment in pregnancy among the intervention group. Although Balami, et al. [22] focused on the impact of knowledge and behavioral skills in their intervention group,
Discussion
This systematic review primarily aimed to investigate the effectiveness of interventions for improving the uptake of IPT for malaria control among pregnant women in SSA. However, considering the comprehensive evidence provided by the primary aim of this review, establishing the effectiveness of IPT for malaria control among pregnant women in SSA and the level of uptake and compliance with IPT for malaria control among pregnant women in SSA is imperative as the secondary objectives of this review.
Three studies were in line with the secondary objectives of this study [20,21,23]. From the structured literature review, a total of 3988 women participated in these studies. Studies included in the review adopted a one-arm intervention and control group in comparing the effectiveness of the interventions and uptake of IPTp [20,21-23]. [20] demonstrated the relationship between IPTp coverage and uptake, which subsequently recorded an increased IPTp uptake. Another study investigated the knowledge-based effect using a model designed for information motivation and behavioral skills (IMB) [22] with unclear evidence of improved IPT uptake. However, several publications have considerably affirmed the opinion that the knowledge of methods of malaria infection prevention in pregnancy is an integral aspect of care [27,28,29]. Furthermore, Kinyina, et al. [21] and Gies, et al. [23] clearly reported the effectiveness of community-based interventions for improving IPTp uptake.
Three of the studies reported policies and guidelines adopted by their country in increasing uptake and good harmonization of doses of IPTp with a positive impact [20,21,23]. Research has shown that strong partnerships among countries exist between the stakeholders is a step in addressing the barriers to IPTp uptake [30,31]. Based on this array of opinions, misunderstanding of these guidelines, lack of supplies, and inappropriately defined targets are liable to impede intervention measures among groups [32,33].
Considering further findings of this review, it is observed that pregnant women attending ANC at multi-centres were involved in health promotional activities in three studies [20,21]. Nonetheless, a recent Turkish systematic review by Rogerson, et al. [30] revealed that women’s malaria prevention assessments when using IPTp demonstrated a positive influence of community promotional activity, resulting in an increased uptake of SP among Turkish women attending ANC. This is important because, according to Arnaldo, et al. [31], malaria in pregnancy remains a devastating condition that can lead to mortality and several complications.
The findings of this review revealed that three studies reported increased uptake of IPTp-Sp doses among pregnant women following promotional activity [20,21,23]. Notably, according to several publications [6,14,34], low attendance of ANC in conjunction with a low proportion of pregnant women eligible to receive IPTp-SP at healthcare facilities shows substantial gaps which could result in the inability of facilities to provide IPTp3. Conversely, drops in coverage between IPTp1 and subsequent doses are particularly concerning and there is pertinence for action [35].
Further information in terms of the outcomes of the RCTs posited that two studies revealed that about one-quarter of the women who participated in the studies had their first ANC visit during the third trimester [21,23]. This could be due to women in the studies having incorrect information and knowledge about ANC. This finding is in line with several maternal and child studies conducted in Africa [27-29,36]. However, it is contrary to a finding by Bardaj, et al. [36] that explained the causes and problems of ANC visits among women in pregnancy as significantly poor access to ANC. The methodological quality of this review was an assessor of the outcome-based approach adopted in appraising the completeness of systematic reviews. The included studies were of fair quality [21] and of very high and very high quality [20,23,22], judging from the risk of bias.
This review revealed an association between ANC attendance and uptake of IPTp-SP in three of the studies. According to Desai, et al. [27] in a Gambian study, scheduled ANC attendees have a clear access to being exposed to information on the adoption of measures that would prevent them from having harmful pregnancy outcomes. This indicates that there is an association between ANC and IPTp uptake. Thus, focusing on improving ANC attendance could help to improve IPT uptake.
Two of the studies in this review suggested that promotion activities were associated with a more than two-fold increase in complete ANC attendance in women who delivered during the low malaria transmission season for adults and adolescents [21,23]. Conversely, one of the studies showed that among the women in Burkina Faso who delivered during the high transmission season, the effect of the promotion was unclear in adults and absent in adolescents [23]. Consequently, this could suggest that the level of uptake of IPTp-SP is significantly less among adolescent mothers than among adult mothers who delivered or conceived during the season of high transmission; however, it did not differ between the areas of non-promotion and promotion [23]. A study conducted in Kenya by Kuile, et al. [38] reported that the age of women has an effect on the uptake of SP, which is in line with the findings of this study. With overwhelming corroboration of findings with this review, a study conducted in Malawi revealed that the uptake of IPTp among pregnant women in a survey increased from 41.5% to 82.9% in country-wide coverage as a result of promotional activities [28]. In addition, a systematic review involving 2198 participants evaluating SP distribution in the community by health workers showed that a community approach to IPT in pregnancy was effective and led to increased attendance of antenatal care among women with women complying with appointments made by health care providers [39,22]. In addition, explored information on the knowledge and motivation skills of participants in a study towards malaria prevention in pregnancy with IMB skills. Information from this study suggests that knowledge of these prevention methods improves participants’ wide-skilled practice with positive motivation skills (i.e., the superiority of the IMB model) towards IPTp. Another systematic review by Menéndez, et al. [40] reported the effect of malaria prevention methods and ANC among women of childbearing age and found that increasing educational methods on malaria prevention improved ANC utilization of participants explored in the studies of the review. Based on the findings of these studies, women in pregnancy and women of childbearing age in general should participate often in periodic health examinations and ANC services.
Evidence and findings from a study are pertinent to be subjected to a quality assessment of its overall methodology [41]. Based on this study, with differing and contrasting parameters in baseline characteristics of participants, such as parity, sample size of women, and statistical analysis employed, however, conducting the meta-analysis of the study was problematic and impossible. The quasi-homogeneity of this study was also enhanced with differing units in numerical data representation in the participants’ baseline demographic characteristics. Overall, the above discussed were critical considerations taken in ensuring the quality of evidence reported in this review.
Conclusion
Our analysis showed the effectiveness of community-based promotional activities in improving the uptake of IPTp-Sp doses among pregnant women in SSA. This evidence and findings would be essential for policy-makers and health agencies in SSA to further find effective means to apply this in the SSA region. However, considering the findings of this review, it is imperative and vital for future research to examine RCTs on the perception and uptake of ANC in and before pregnancy among women in Africa. This is due to the fact that there is a gap in the literature and it would provide a wider gap for retrospective and prospective follow-up of participants in existing studies. Meanwhile, with the paucity of evidence on post and pre-antenatal among pregnant women, data on it would be pertinent for the future. Also, the formulation of policies that would position pregnant women as a high-risk group is essential to facilitate actions and service delivery when the need occurs [41]. Furthermore, with this implication of prioritized consideration of women in pregnancy, scaling health interventions by health ministries and concerned organizations is necessary to improve intervention measures in the adoption of IPT measures and approaches.
Existing reviews show that
- Pregnant women’s uptake of intermittent preventive treatment continues to improve.
- Antenatal care facilities incorporating IPT uptake in the regimen of care among pregnant women.
- Studies show differences in uptake and harmonization of doses of IPTp.
This study will add the following
- Improve and inform policymakers in sub-saharan Africa on IPT uptake among Pregnant.
- Also, this study will add to the existing literature to aid future researchers in building empirical evidence for their findings.
- Pregnant women taking intermittent preventive treatment will through the findings of this study understand the uptake and harmonization of doses of IPTp.
Declarations
Availability of data and materials: The Data set from the study is available from the corresponding author upon request.
Final approval of the manuscript: All authors
Authors Contributions
Chukwuma Ernest Egbujor: Conceptualization, Project design, and administration, investigation, methodology, writing- Original Draft preparation, Writing - Review editing.
David Chinaecherem Innocent: Data Curation, methodology, investigation formal analysis, writing- Original Draft preparation, Writing - Review editing.
Uchechukwu Madukaku Chukwuocha: Software, validation, writing- Original Draft preparation, Writing - Review editing.
John Chigozie Ekenze: Validation, writing- Original Draft preparation, Writing - Review editing.
Ugonma Winnie Dozie: Supervision, Investigation, writing- Original Draft preparation, Writing - Review editing.
Chiagoziem Ogazirilem Emerole: Methodology, writing- Original Draft preparation, Writing - Review editing.
Igiri Vivian Chika: Data curation, methodology, formal analysis, writing- Original Draft preparation, Writing - Review editing.
Nanush Damarlapally: Supervision, Investigation, writing- Original Draft preparation, Writing - Review editing.
Stanley Chinedu Eneh: Data curation, methodology, investigation formal analysis, writing- Original Draft preparation, Writing - Review editing.
Uzochukwu Godswill Ekeleme: Supervision, Investigation, writing- Original Draft preparation, Writing - Review editing.
- World Malaria Report. Geneva: World Health Organization; 2021. License: CC BY-NC-SA 3.0 IGO.
- World Health Organization. Global Malaria Programme: pregnant women and infants. 2019. http://apps.who.int/malaria/pregnantwomenandinfants.html.
- McMurry C. Situation of Children, Youth and Women in the Solomon Islands: Update. Honiara: Solomon Islands Government and UNICEF, 2014.
- Center for Disease Control and Prevention. CDC: Malaria vaccine: CDC position paper. (PDF). Weekly Epidemiological Record, 2011; 91(4):33-52.
- Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, Flenady V, Frøen JF, Qureshi ZU, Calderwood C, Shiekh S, Jassir FB, You D, McClure EM, Mathai M, Cousens S; Lancet Ending Preventable Stillbirths Series study group; Lancet Stillbirth Epidemiology investigator group. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016 Feb 6;387(10018):587-603. doi: 10.1016/S0140-6736(15)00837-5. Epub 2016 Jan 19. PMID: 26794078.
- Innocent DC, Emerole CO, Ezejindu CN, Dozie UW, Obani SI, Uwandu-Uzoma AC, Nwaokoro CJ, Udeh MU, Eneh SC, Uwaezuoke AC, Iwuji KM. Examination of Common Occupational Hazards among Healthcare Workers in a University Healthcare Center in Southeastern Nigeria. Health. 2022; 3:14(8);833-52.
- World Health Organization. Guidelines for the Treatment of Malaria.Geneva: World Health Organization, 2006.
- White NJ, Breman JG. Malaria. In: Fauci AS, Braunwald E, Kasper DL, et al., editors. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill. 2008; 28: 1280–1293.
- Falade CO, Yusuf BO, Fadero FF, Peters PJ, Cyril MC, Olushola ME, Adegoke RD. Intermittent preventive treatment with sulphadoxine-pyrimethamine is effective in preventing maternal and placental malaria in Ibadan, southwestern Nigeria. Malarial Journal. 2017; 6: 88.
- Ducarme G, Thuillier C, Wernet A, Behrens CB, Micek MA. Malaria in pregnant woman masquerading as HELLP syndrome. American Journal of Perinatal. 2016; 28: 1280-1293 doi: 10.1055/s-0029-1234035.
- Innocent DC, Vasavada A, Eneh SC, Uwaezuoke AC. Systematic review evidence on the factors influencing teenage mothers’ utilization of maternal health services in Sub-Saharan Africa. ACADEMIC JOURNAL. 2023.
- Ofori M, Ansah E, Agyepong I, Ofori-Adjei D, Hviid L, Akanmori B. Pregnancy-associated malaria in a rural community of ghana. Ghana Med J. 2009 Mar;43(1):13-8. PMID: 19652749; PMCID: PMC2709171.
- World Health Organization. WHO policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP) (No. WHO/HTM/GMP/2014.4). World Health Organization. 2014. https://www.who.int/malaria/publications/atoz/iptp-sp-updated-policy-brief [Accessed 20 March. 2023]
- Dozie UW, Ezeala OV, David CI, Dozie KCN, Chukwuocha UM, Iwuala CC, Osuoji NJ, Okoro CC, Chukwu OR, Eneh SC, Dozie INS. Factors associated with health seeking delay in the screening of cervical cancer among women in Imo state, south Eastern Nigeria. Cancer Treat Res Commun. 2023 Sep 29;37:100765. doi: 10.1016/j.ctarc.2023.100765. Epub ahead of print. PMID: 37806167.
- World Health Organization. WHO Evidence Review Group on Intermittent Preventive Treatment (IPT) of malaria in pregnancy. WHO Headquarters, Geneva, 9-11 November 2013. Draft Recommendations on Intermittent Preventive Treatment in Pregnancy (IPTp).http://www.who.int/malaria/mpac/mpac_sep13_erg_ipt_malaria_pregnancy_report.pdf [Accessed 20 March. 2023]
- Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. Journal of the Medical Library Association: JMLA. 2018; 106(4):420. [Accessed 20 March. 2023].
- Aromataris E, Riitano D. The Joanna Briggs Institute Systematic Review, Step by Step Constructing a Search Strategy and Searching for Evidence -A guide to the Literature Search for a Systematic Review. AJN, 2014; 114(5). https://alliedhealth.ceconnection.com/files/ctingaSearchStrategyandSearchingforEvidence-1430415746583.pdf [Accessed 20 March. 2023]
- Higgins J, Altman D. Assessing Risk of Bias in Included Studies. In: J. Higgins, and S. Green (eds). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley & Sons Ltd. 2008; 187-241. [Accessed 20 March. 2023]
- University of Canberra. Systematic Reviews in Health. Available at https://canberra.libguides.com/systematic/extract 2021. [Accessed 20 March. 2023]
- Gutman JR, Stephens DK, Tiendrebeogo J, Badolo O, Dodo M, Burke D, Williamson J, Vibbert K, Youll SJ, Savadogo Y, Brieger WR. A cluster randomized trial of delivery of intermittent preventive treatment of malaria in pregnancy at the community level in Burkina Faso. Malar J. 2020 Aug 5;19(1):282. doi: 10.1186/s12936-020-03356-9. PMID: 32758233; PMCID: PMC7409482.
- Kinyina A, Lyimo G, Chamos S. Impact of Community Intermittent Preventive Treatment in Pregnancy (C-IPTp) approach on the uptake of IPTp3+: a randomized controlled trial in Karagwe, Tanzania. South Sudan Medical Journal. 2020; 15 (4): 175-177.
- Balami AD, Said SM, Zulkefli NAM, Bachok N, Audu B. Effects of a health educational intervention on malaria knowledge, motivation, and behavioural skills: a randomized controlled trial. Malar J. 2019 Feb 20;18(1):41. doi: 10.1186/s12936-019-2676-3. PMID: 30786906; PMCID: PMC6381678.
- Gies S, Coulibaly SO, Ky C, Ouattara FT, Brabin BJ, D’Alessandro U. Community-based promotional campaign to improve uptake of intermittent preventive antimalarial treatment in pregnancy in Burkina Faso. Am J Trop Med Hyg. 2009 Mar;80(3):460-9. PMID: 19270299.
- Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003 Aug;83(8):713-21. PMID: 12882612.
- Higgins JP, Ramsay C, Reeves BC, Deeks JJ, Shea B, Valentine JC, Tugwell P, Wells G. Issues relating to study design and risk of bias when including non-randomized studies in systematic reviews on the effects of interventions. Res Synth Methods. 2013 Mar;4(1):12-25. doi: 10.1002/jrsm.1056. Epub 2012 Sep 25. Erratum in: Res Synth Methods. 2013 Sep;4(3):287-9. PMID: 26053536.
- Jarde A, Losilla JM, Vives J. Methodological quality assessment tools of non-experimental studies: a systematic review. Annals of Psychology. 2012; 28(2): 617–628.
- Desai M, Gutman J, L’lanziva A, Otieno K, Juma E, Kariuki S, Ouma P, Were V, Laserson K, Katana A, Williamson J, ter Kuile FO. Intermittent screening and treatment or intermittent preventive treatment with dihydroartemisinin-piperaquine versus intermittent preventive treatment with sulfadoxine-pyrimethamine for the control of malaria during pregnancy in western Kenya: an open-label, three-group, randomised controlled superiority trial. Lancet. 2015 Dec 19;386(10012):2507-19. doi: 10.1016/S0140-6736(15)00310-4. Epub 2015 Sep 28. PMID: 26429700; PMCID: PMC4718402.
- Hennessee I, Chinkhumba J, Briggs-Hagen M, Bauleni A, Shah MP, Chalira A, Moyo D, Dodoli W, Luhanga M, Sande J, Ali D, Gutman J, Lindblade KA, Njau J, Mathanga DP. Household costs among patients hospitalized with malaria: evidence from a national survey in Malawi, 2012. Malar J. 2017 Oct 2;16(1):395. doi: 10.1186/s12936-017-2038-y. PMID: 28969643; PMCID: PMC5625606.
- Boudová S, Divala T, Mawindo P, Cohee L, Kalilani-Phiri L, Thesing P, Taylor TE, Laufer MK. The prevalence of malaria at first antenatal visit in Blantyre, Malawi declined following a universal bed net campaign. Malar J. 2015 Oct 29;14:422. doi: 10.1186/s12936-015-0945-3. PMID: 26510414; PMCID: PMC4625940.
- Rogerson SJ, Chaluluka E, Kanjala M, Mkundika P, Mhango C, Molyneux ME. Intermittent sulfadoxine-pyrimethamine in pregnancy: effectiveness against malaria morbidity in Blantyre, Malawi, in 1997-99. Trans R Soc Trop Med Hyg. 2000 Sep-Oct;94(5):549-53. doi: 10.1016/s0035-9203(00)90083-x. PMID: 11132387.
- Arnaldo P, Cambe MI, Magaço A, Chicumbe S, Rovira-Vallbona E, Rosanas-Urgell A, Enosse SM. Access to and use of preventive intermittent treatment for Malaria during pregnancy: A qualitative study in the Chókwè district, Southern Mozambique. PLoS One. 2019 Jan 24;14(1):e0203740. doi: 10.1371/journal.pone.0203740. PMID: 30677039; PMCID: PMC6345468.
- Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U, Battle K, Moyes CL, Henry A, Eckhoff PA, Wenger EA, Briët O, Penny MA, Smith TA, Bennett A, Yukich J, Eisele TP, Griffin JT, Fergus CA, Lynch M, Lindgren F, Cohen JM, Murray CLJ, Smith DL, Hay SI, Cibulskis RE, Gething PW. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2015 Oct 8;526(7572):207-211. doi: 10.1038/nature15535. Epub 2015 Sep 16. PMID: 26375008; PMCID: PMC4820050.
- Williams LL. Malaria eradication in the United States. American Journal of Public Health, Nations Health. 2013; 53: 17–21.
- Briand V, Badaut C, Cot M. Placental malaria, maternal HIV infection and infant morbidity. Ann Trop Paediatr. 2009 Jun;29(2):71-83. doi: 10.1179/146532809X440699. PMID: 19460261.
- Orton LC, Omari AA, Parise ME, Newman RD. Drugs for treating uncomplicated malaria in pregnant women. Cochrane Database Systematic Reviews. 2018; 4 CD004912.
- Bardají A, Bassat Q, Alonso PL, Menéndez C. Intermittent preventive treatment of malaria in pregnant women and infants: making best use of the available evidence. Expert Opin Pharmacother. 2012 Aug;13(12):1719-36. doi: 10.1517/14656566.2012.703651. Epub 2012 Jul 9. PMID: 22775553.
- Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, Newman RD. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007 Feb;7(2):93-104. doi: 10.1016/S1473-3099(07)70021-X. PMID: 17251080.
- Guyatt HL, Snow RW. A Systematic Review on the epidemiology and burden of Plasmodium falciparum-related anemia among pregnant women in sub-Saharan Africa. American Journal of Tropical Medical Hygiene. 2011; 64(1):36–44. doi: 10.4269/ajtmh.64.36.
- Menéndez C, Romagosa C, Ismail MR. An autopsy study of maternal mortality in Mozambique: the contribution of infectious diseases. PLoS Med. 2018; 5: e44.
- Neyarapally GA, Hammad TA, Pinheiro SP, Iyasu S. Review of quality assessment tools for the evaluation of pharmacoepidemiological safety studies. BMJ Open. 2020; 2(5): e001362.
- USAID. President’s Malaria Initiative; Malawi Operational Plan FY17. 2017. https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy17/fy-2017-malawi-malaria-operational-plan.pdf?sfvrsn=6.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
