Archives of Preventive Medicine
A Prospective Study to Evaluate the Prevalence of Complementary and Alternative Medicine among Cancer Patients in India
AR Bansal1*, Kapil Vats2, Joy Bansal3, Durgesh Goyal2 and Harsha Kamalhans4
1Sr. Professor & Unit Head, Department of Surgery, Pt. Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, (124001) Haryana, India
2Sr. Resident, Department of Surgery, Pt. Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, (124001) Haryana, India
3Jr. Resident, Department of Surgery, MMU Solan, Himachal Pradesh, India
4Jr. Resident, Department of Surgery, Pt. Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, (124001) Haryana, India
Cite this as
Bansal AR, Vats K, Bansal J, Goyal D, Kamalhans H. A Prospective Study to Evaluate the Prevalence of Complementary and Alternative Medicine among Cancer Patients in India. Arch Prev Med. 2025; 10(1):001-005. DOI: 10.17352/apm.000037Copyright
© 2025 Bansal AR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: Cancer is a major public health problem and remains one of the leading causes of death. Most patients turn to Complementary and Alternative Medicine (CAM) when they are in the terminal stage and Conventional Medicine (CM) has not completely cured them. CAM majorly includes herbal medicine, spiritual therapy, and daily supplements, among many other things.
Methods: A total of 215 diagnosed cancer patients were assessed, amongst other things like age, literacy, income, etc., and also particularly any benefits and side effects of CAM, and whether they are still using CAM or not.
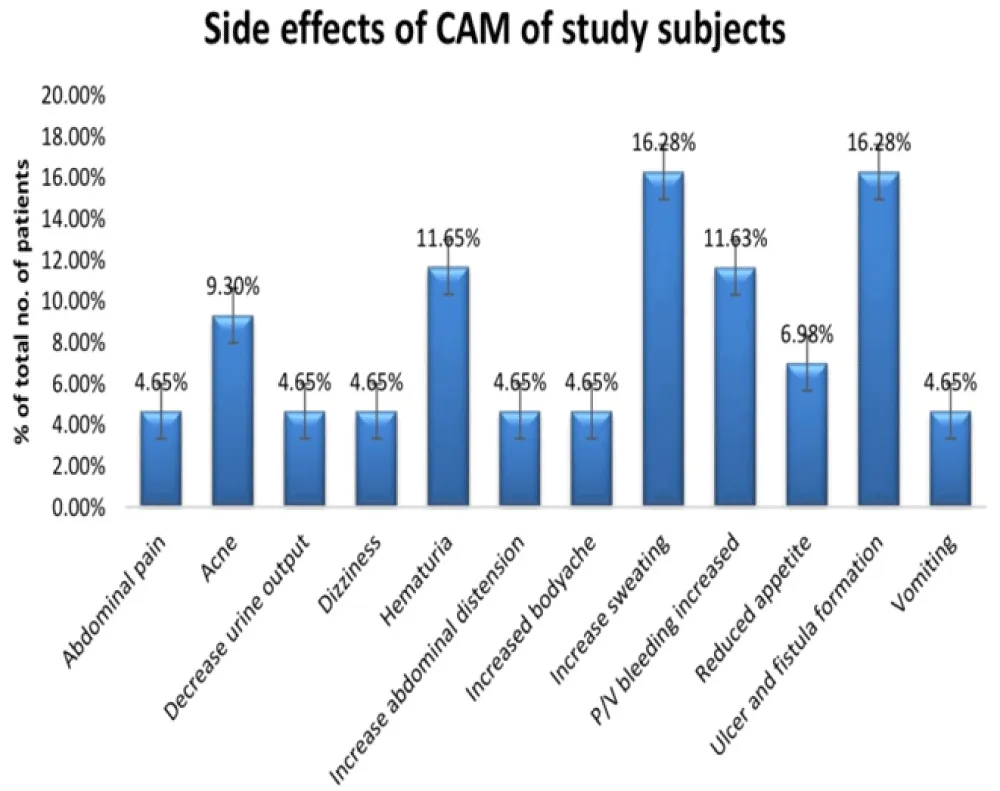
Results: A handful of 19 patients benefited from CAM amongst the 116 participants who were using CAM, while 43 of the CAM users reported side effects like ulcer and fistula formation, increased sweating, hematuria, acne, etc.
Conclusion: Despite significant advances with CM, there is increasing use of CAM in the belief of a permanent cure, particularly amongst the terminally ill cancer patients.
Introduction
Cancer is a leading cause of death worldwide, accounting for an estimated 7.6 million deaths in 2008 and 9.6 million deaths in 2018 [1,2]. Deaths from cancer globally are projected to continue to increase to over 13.1 million in 2030 [2]. About 70% of deaths from cancer are reported in low- and middle-income countries.
Early detection of cancer and management of patients can also reduce the cancer burden. There are high chances of a cure for many cancers if they are diagnosed early and treated properly [1]. There is a specific treatment regimen for every cancer type, which comprises one or more modalities like surgery, radiotherapy, and chemotherapy [2]. Despite remarkable advances achieved by conventional medicine, there has been an increasing growth in interest in the use of Complementary and Alternative Medicine (CAM), even in developed Western countries [3]. Many adverse effects are reported by conventional therapies such as surgery, chemotherapy, radiotherapy, and hormone therapy. The World Health Organization (WHO) defines CAM as “A comprehensive term used to refer to both traditional medical systems such as traditional Chinese medicine, Indian Ayurveda, Arabic Unani medicine, and to various forms of indigenous medicine” [4].
The integration of CAM into the national health systems is always a subject of constant debate [5]. As per the recommendation of WHO, there is a need to investigate national integration policies of complementary and alternative therapies in the national health systems; safety, efficacy, and quality of these therapies; access to these therapies; and rational use by professionals and CAM users. Despite the unproven safety and efficacy of Complementary and alternative medical (CAM) practices, these are increasingly becoming popular worldwide, and many cancer patients have turned to CAM with the hope of finding a treatment for their illness, and to make themselves feel better [6,7]. Over the past 15 years, the usage of CAM has increased exponentially. It has gained medical, economic, and sociological importance [7]. However, little is known about the use of CAM in cancer patients specifically. As the use of traditional remedies and herbs is well known and relatively common in our country, many cancer patients use CAM as a single therapy or in combination with standard therapy. But, there is a lack of studies in India studying the prevalence of the use of CAM in cancer patients. Thus, the present study aimed to determine the prevalence of CAM use, the reason for using CAM, the perceived effectiveness, as well as the continuance of its use.
Material and method
The present prospective observational cross-sectional study comprised 215 diagnosed cancer patients. Patients who were unable to understand verbal or written instructions to complete the questionnaire (a semi-structured standardized interview schedule, protocol was approved by the institutional ethics committee) were excluded from the study, as also pregnant women along patients with any neurological disorder, like schizophrenia or other psychiatric disorders. Informed and written consent was taken from all the participants who were willing to participate in the study. The present study is well within the ethical norms and hence, as per the Institute Ethics Committee. All participants were assessed with a detailed history and clinical examination by probing various questions about the disease, stage, their age, sex, marital status, education, employment, income, benefit, and side effects of CAM, and do they still use CAM or not, and the expenditure on CAM.
Observations and results
The mean age of the participants was calculated to be 52.05(13.72) years. The majority of participants (26%) belonged to the 41-50 years age group, followed by 25.5% participants in the 51-60 years age group. Noticeably, only 6.5% participants were found in both the < 30 years and > 70 years age groups. More than 75% of the participants were married.
32% participants had a high school qualification, 9.3% participants had a college education, and only 4.6% participants had a professional degree; 28.8% participants were illiterate. Compared to participants who did not use CAM, the participants who opted for CAM had a significant statistical difference in terms of education (p = 0.019).
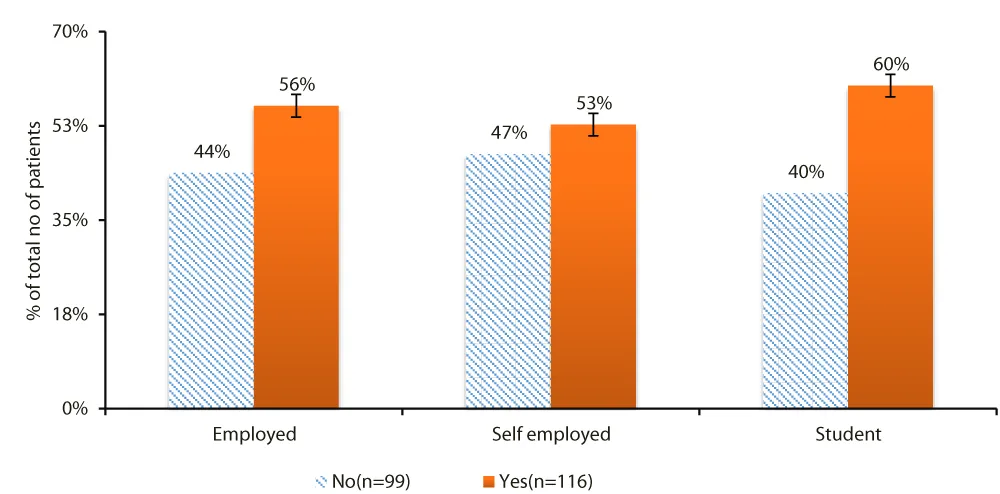
67.9% participants were self-employed, 29.7% participants were employed with the public or private sector, and 2.3% participants were dependent on their families for financial support (Figure 1).
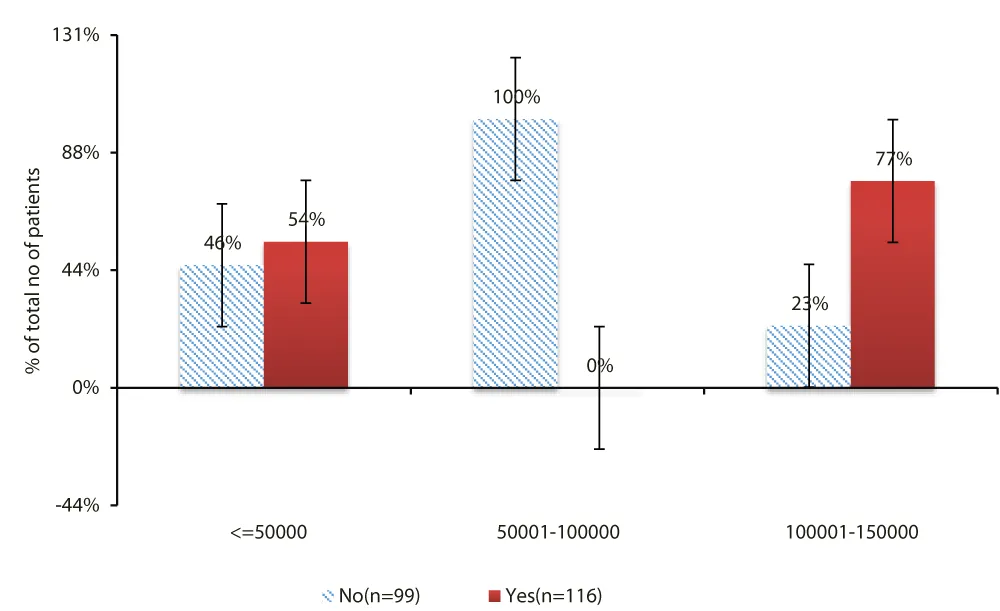
The participants who opted for CAM had a comparably higher monthly income than those who did not use CAM (p = 0.004). Mean monthly income of participants ranged from ₹27618/- to ₹ 33301/- (Figure 2).
8.8% participants had stage 2 cancer, while 6.9% participants had stage 3 cancer, followed by 4.1% participants in stage 4. Surprisingly, in 75.8% participants staging of cancer was not known, i.e., Tx(since all these patients had already taken treatment elsewhere for their cancer disease and had now reported with advanced disease). In the present study primary treatment rendered in 51.1% participants was chemotherapy, in 45.5% participants, and in 3.2% participants.
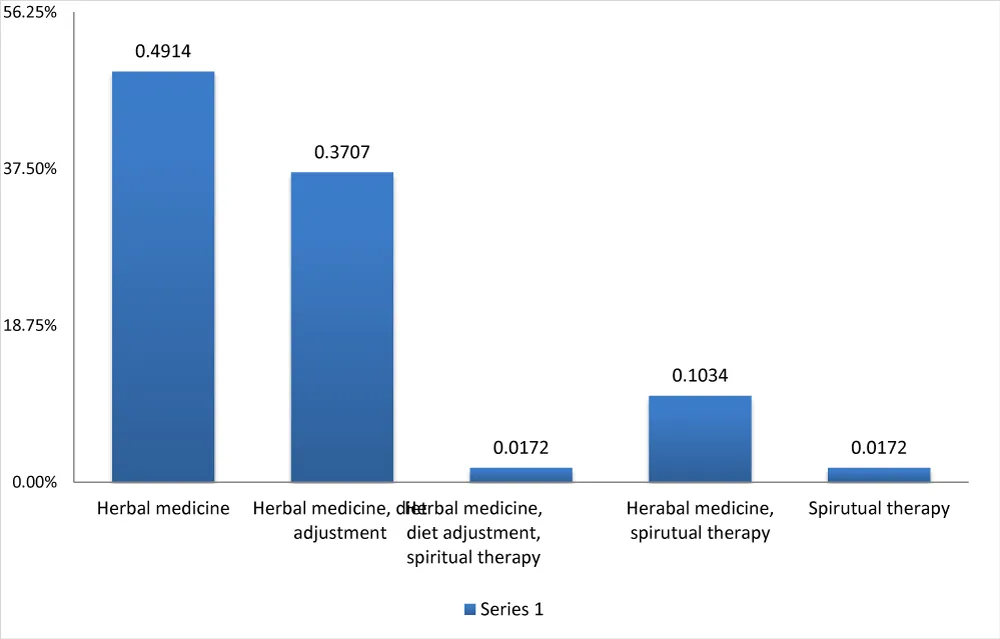
Out of a total of 215 participants, a total of 116 (53.9%) chose Complementary and Alternative Medicine (CAM). 49.1% participants were using herbal medicine, whereas 37% participants opted for herbal medicine with diet adjustment. 10.3% participants were using herbal medicine along with spiritual therapy, while while1.72% participants went with herbal medicine along with diet adjustment and spiritual therapy. Only 1.7% participants picked spiritual therapy solely (Figure 3).
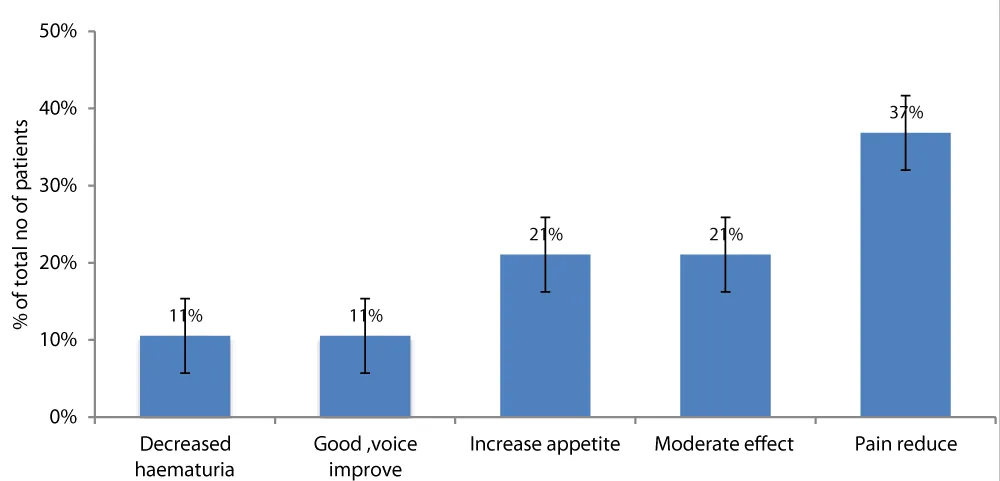
A total of 16.3% (n = 19) reported benefit from CAM. 7 participants reported reduced pain, followed by 4 who had increased appetite, 4 showed moderate effect on their quality of life, 2 had decreased hematuria, and 2 had good voice improvement (Figure 4).
37% (n = 43) reported side effects of CAM, which is highly significant (p < 0.05). The side effects included increased sweating in 7 participants, followed by 7 participants who presented with ulcer and fistula formation,5 participants reported hematuria, 5 participants reported with increased P/V bleeding and rest of the side effects included reduced appetite, abdominal pain, acne, decreased urine output, dizziness, increase abdominal distension, increase body ache, vomiting. Mean CAM expenditure of participants was ₹ 8157.76/- (Figure 5).
On further enquiry from the patients who were using CAM, more than 90% of the patients could not identify the doctor/person as to whether he was qualified to give any drugs under Ayurveda, Unani, or homeopathy.
Discussion
Cancer has emerged as a major public health problem in developing countries as well as developed nations. India is in an epidemiological transition phase, and cancer is now one of the leading causes of morbidity and mortality. People often turn to Complementary and Alternative Medicine (CAM) when they have a long-lasting problem that Conventional Medicine (CM) has not completely cured. CAM is a group of diverse medical and healthcare systems, practices, and products that are not generally considered part of conventional medicine [3].
Treatment with CM has caused significant advances in the prevention, detection, and treatment of cancer. However, many participants choose CAM over CM in the hope of maintaining wellness and curing the disease. The decision to use CAM is typically influenced by factors like poor doctor–patient communication, emotional effect of a cancer diagnosis, perceived severity of conventional treatment side-effects and strong beliefs in holistic healing and the mind–body–spirit connection. CM focuses on curative aspects without focusing on the social, psychological, and spiritual needs of the patient. CAM therefore fills this void. It has been estimated that two-thirds of the world’s population seek healthcare from sources other than conventional medicine [8]. However, many questions remain regarding the proper use of CAM, particularly regarding dosage and contaminants.
Blind use of CAM by participants may confuse their treating doctors, which may affect diagnostic and treatment decisions, resulting in misleading or unknown treatment outcomes [3]. There is no evidence claiming that CAM is more effective than CM, but public opinion and interest in CAM are strong and growing. There are only a few clinical studies to evaluate the prevalence of CAM and the efficacy of various CAM therapies tried by Indian participants. It is still a question whether evidence-based CAM, if integrated properly with mainstream medicine, can play an important role in cancer management.
The mean age of the participants in the present study was 52.05(3.72) years. Concordant results were found by Mujar NM, et al. [9] and Ezeome NE, et al. [10] in their study, with the median age being 53 years (23 to 74 years) and 52.3 years, respectively. The mean age of participants in the present study who were either using CAM or were on conventional cancer therapy was comparable (p > 0.05). This is in contrast to Broom A, et al. [6] where the mean age of the TCAM (traditional CAM) users was significantly higher than that of non-TCAM (non-traditional CAM) users (p < 0.05). Also, Bahall M, et al. [5] reported that age was the only socio-demographic variable associated with CAM use, as increasing age was associated with increased use of CAM. India confronts very specific social, cultural, and economic issues when it comes to addressing cancer (e.g., geographical diversity, class, and caste structure).
Low socioeconomic status and illiteracy also contribute to advanced stages of disease [6]. Bahall M, et al. [5] mentions that marital status was comparable between CAM and non-CAM groups, so marital status was not a useful predictor of CAM use. More than 75% of the participants were married in the present study. The majority of participants (32.0%) studied up to high school. Compared to participants who did not use CAM, the participants who opted for CAM had significant statistical difference in terms of education (p < 0.05 whereas, Bahall M, et al. [5] reported that among CAM users, majority had education up to secondary school; education status between two groups (CAM and non-CAM users) was comparable (p > 0.05). Mujar NM, et al. [9] found that CAM use was seen mainly amongst the low educational status participants, but education status between the two groups was comparable [11-16].
Mean monthly income of the participants in the present study ranged from ₹27618.6 to ₹33301.98. Compared to participants who did not use CAM, the participants opting for CAM had comparable higher monthly income (p < 0.05). Mujar NM, et al. [9] mentioned that most of the CAM users had household income > RM 3000 (1 Malaysian Ringgit = ₹17.8 in 2012) and the monthly income distribution was comparable between CAM and non-CAM users. Ezeome NE, et al. [10] reported that most of the CAM users belonged to low socioeconomic status, but the difference between the two groups on the basis of income was comparable 67.9% participants in the present study were self-employed, 29.7% were employed, and 2.3% were students. Compared to participants who did not use CAM, the participants who opted for CAM had comparable employment status distribution (p > 0.05). As per a study by Bahall M, et al. [5] among CAM users majority were unemployed (p > 0.05). Mujar NM, et al. [9] also reported majority of the CAM users were unemployed (p > 0.05)
Patients were influenced to use or introduced to CAM by family, friends, religious groups, mass media, in-hospital personnel, CAM practitioners, and health personnel outside of a hospital [5]. Social media and mass media also play a role in increasing the use of CAM. In the present study, the source of information for the majority of participants (54.3%) was family members, followed by friends (34.4%), and the rest of the sources of information included other cancer patients, the internet, magazines, newspapers, and books. Patient awareness/information about CAM usage was obtained from friends (69.3%), followed by family members, in a study by Bahall M, et al. [5]. Similar results were reported by Mujar NM, et al. stated that CAM users started using CAM after being influenced by family members and friends [9].
The majority of Indian cancer participants have late-stage incurable diseases when first diagnosed, mainly because of illiteracy, low socioeconomic status, lack of knowledge and awareness, lack of medical facilities, etc. Only 8.8% participants had stage 2 cancer, followed by 6.9% participants with stage 3 cancer. This was in contrast to a study conducted by Mujar NM, et al. [9] found that the majority of patients had stage II cancer, followed by stage III cancer.51.1% participants received chemotherapy followed by surgery in 45.5%. Ezeome NE, et al. [10] quoted similar results that at the time of the interview, 50.6% were receiving chemotherapy, 20.6% underwent surgery, and 3.8% were put on symptomatic palliative therapy.
India is a multiethnic and multicultural country with people having strong traditional beliefs and practices. Socio-cultural beliefs and practices influence the help-seeking behavior of cancer participants, which leads them to use CAM along with CM. The usage of CAM in participants has increased over the past 10–15 years and has gained economic, medical, and sociological importance. Use of CAM in the Indian community is quite common, as 53.9% participants were using CAM, which is almost comparable with the world literature. Mujar NM, et al. [9] had 46.5% participants as CAM users, while Chaturvedi P, et al. [4] found that 38% had visited CAM practitioners. As per Kumar D, et al. [3] overall CAM use was among 38.7% participants, and Bahall, et al. 13 reported usage by 39.1% participants.
CAM includes the use of herbs, spiritual therapies, dietary supplements, biofeedback, hypnosis, acupuncture, Ayurveda, homeopathy, naturopathy, Chinese medicine, chiropractic, massage, Tai chi, yoga, electromagnetic therapy, kinesiology, Reiki, and qigong. 49.1% participants were consuming herbal medicine, followed by 37% participants availing herbal medicine along with diet adjustment. Kumar D, et al. [3] and Broom A, et al. [6] reported Ayurveda to be the most common CAM therapy in use by cancer participants, followed by Homeopathy, Meditation, Acupuncture, and Reiki. Bahall M, et al. [5] reported medicinal herbs (94.2%) and spiritual therapy as the most common types of CAM used. A total of 19 out of 116 participants (16.3%) mentioned benefited from CAM. Bahall M, et al. [5] Ezeome NE, et al. [10] and Yun YH. et al. [1] mentioned that there was no association between the type of cancer and CAM users and found that CAM did not provide any definite survival benefit or improved health-related quality of life in terminally ill cancer patients.
Many CAM therapies lack a scientific basis and are of questionable safety and efficacy, which may lead to major health consequences, delayed treatment, disease complications, and even death. There is a possibility of herbal toxicity and herb-herb and herb-drug interactions. CAM-anticancer drug interactions are responsible for substantially more unexpected toxicities of chemotherapeutic drugs and possible under-treatment of cancer participants [5]. Forty-three out of 116 participants (37%) reported side effects of CAM, like increased sweating and ulcer, and fistula formation; followed by hematuria, P/V bleeding increased, reduced appetite, abdominal pain, acne, decreased urine output, dizziness, increased abdominal distension, increased body ache, and vomiting. Ezeome NE, et al. [10] reported that 21.2% participants had anorexia, nausea and vomiting, weakness, malaise, generalized body discomfort, diarrhoea/mucoid stool, bleeding from wound and urine, cough, worsened stomach upset, skin excoriations, and constipation with frequent urination.
As stated above, CAM has no scientific or proven benefit; the outcome results are only subjective, and the purpose of the study was to make people aware of the benefits/side effects of CAM instead of conventional practice.
Conclusion
CAM prevalence is increasing day by day despite significant advancements in conventional medicine. There is high usage of CAM, particularly during the palliative care of cancer patients. Educated and higher-income group participants are more inclined to use CAM. Herbal medicine was the most commonly used CAM, but the paucity of professional CAM supervision, low disclosure rates, lack of meaningful advice from conventional medicine providers, and poor monitoring contribute to a major public health problem. The simultaneous practice of CAM and conventional medicine requires greater understanding, communication, and integration of these two forms of treatment. More detailed studies on CAM usage need to be done to better understand the role and implications of CAM in cancer patients, which might help everyone to evaluate a comprehensive approach for the care of cancer patients.
- World Health Organization. Cancer [Internet]. Geneva: World Health Organization; [cited 2019 Jan]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cancer
- World Health Organization. Cancer in India [Internet]. New Delhi: WHO Regional Office for South-East Asia; [cited 2019 Jan]. Available from: http://www.searo.who.int/india/topics/cancer/en/
- Kumar D, Goel NK, Dubey AK, Sarpal SS. Complementary and alternative medicine use among cancer patients in Northern India. South Asian J Cancer. 2016;5(1):8-11. Available from: https://doi.org/10.4103/2278-330x.179689
- Chaturvedi P, Chaturvedi U, Sanyal B. Alternative medicine and cancer patients in less developed countries. Lancet Oncol. 2002;3(1):10. Available from: https://doi.org/10.1016/S1470-2045(01)00615-5
- Bahall M. Prevalence, patterns, and perceived value of complementary and alternative medicine among cancer patients: a cross-sectional, descriptive study. BMC Complement Altern Med. 2017;17:345. Available from: https://doi.org/10.1186/s12906-017-1853-6
- Broom A, Nayar KR, Tovey P, Shirali R, Thakur R, Seth T, et al. Indian cancer patients' use of traditional, complementary, and alternative medicine (TCAM) and delays in presentation to the hospital. Oman Med J. 2009;24(2):99-102. Available from: https://doi.org/10.5001/omj.2009.24
- Yun YH, Lee MK, Park SM, Kim YA, Lee WJ, Lee KS, et al. Effect of complementary and alternative medicine on the survival and health-related quality of life among terminally ill cancer patients: a prospective cohort study. Ann Oncol. 2013;24(2):489-94. Available from: https://doi.org/10.1093/annonc/mds469
- Puataweepong P, Sutheechet N, Ratanamongkol P. A survey of complementary and alternative medicine use in cancer patients treated with radiotherapy in Thailand. Evid Based Complement Alternat Med. 2012;2012:670408. Available from: https://doi.org/10.1155/2012/670408
- Mujar NM, Dahlui M, Emran NA, Hadi IA, Wai YY, Arulanathum S, et al. Complementary and alternative medicine (CAM) use and delays in presentation and diagnosis of breast cancer patients in public hospitals in Malaysia. PLoS One. 2017;12(4):e0176394. Available from: https://doi.org/10.1371/journal.pone.0176394
- Ezeome NE, Anarado AN. Use of complementary and alternative medicine by cancer patients at the University of Nigeria Teaching Hospital, Enugu. BMC Complement Altern Med. 2007;7:28. Available from: https://doi.org/10.1186/1472-6882-7-28
- Adams M, Jewell AP. The use of complementary and alternative medicine by cancer patients. Int Semin Surg Oncol. 2007;4:10. Available from: https://doi.org/10.1186/1477-7800-4-10
- Downer SM, Cody MM, McCluskey P, Wilson PD, Arnott SJ, Lister TA. Pursuit and practice of complementary therapies by cancer patients receiving conventional treatment. BMJ. 1994;309(6947):86-9. Available from: https://doi.org/10.1136/bmj.309.6947.86
- Spadacio C, Barros NF. Use of complementary and alternative medicine by cancer patients: systematic review. Rev Saude Publica. 2008;42(1):158-64. Available from: https://doi.org/10.1590/s0034-89102008000100023
- National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What’s In a Name? [Internet]. Bethesda (MD): NCCIH; [cited 2019 Jan]. Available from: http://nccam.nih.gov/health/whatiscam/
- Ernst E. Complementary cancer treatments: Hope or hazard? Clin Oncol (R Coll Radiol). 1995;7(4):259-63. Available from: https://doi.org/10.1016/s0936-6555(05)80616-8
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
