Global Journal of Rare Diseases
Erythromelalgia: Definition, clinical contexts, differential diagnosis, and therapy. Single case and literature update
1General and Emergency Surgical Clinic, Azienda Ospedaliero-Universitaria “Ospedali Riuniti”, Ancona, Italy
2Physician and “Emergency and Urgency Medicine”, Polytechnic University of Marche, Via Tronto n. 10 / a, 60126, Torrette, Ancona, Italy
Author and article information
Cite this as
Perrotta G, Guerrieri E (2022) Erythromelalgia: Definition, clinical contexts, differential diagnosis, and therapy. Single case and literature update. Glob J Rare Dis. 2022; 7(1): 001-007. Available from: 10.17352/2640-7876.000032
Copyright License
© 2022 Perrotta G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Clinical publications on this morbid condition report as many as 16 different Nav1 7 channel substitutions. They also report more than 40 pharmacological treatments, including agents with sodium channel blocking but nonspecific activity (mexiletine, lidocaine, carbamazepine), anti-neuropathic drugs (gabapentinoids and antidepressants), antidepressant drugs with efficacy on migraines (amitriptyline) vasoactive drugs for the management of hypertension, and analgesics (opioids and ketamine). Current research fails to address all patients’ clinical needs, although it recently suggests new genetic hypotheses yet to be tested and the central importance of genetic counseling, to inform patients and their families about the severity, likely course of symptoms, and risk of complications, and in some cases to guide clinical management. Current findings and the significant morbidity associated with the condition, even in light of the single case presented, highlight the need for mechanism-based therapies to improve clinical outcomes.
Erythromelalgia (or Gerhardt’s or Mitchell’s disease) is a rare disease of functional peripheral arteriopathy that is either primary (or idiopathic) or secondary (to other morbid conditions such as myeloproliferative diseases, hypertension, venous insufficiency, diabetes mellitus, systemic lupus erythematosus, rheumatoid arthritis, gout, lichen sclerosus, spinal cord disease, multiple sclerosis, and rarely by drugs such as nifedipine and bromocriptine); manifests as painful episodic paroxysmal vasodilation primarily in the small arteries of the hands and feet, but may also progress proximally to include the arms and legs, and more rarely to the face and ears). Intense pain, heat, erythema, and redness of the feet or hands are typical symptoms and may last from a few minutes to several hours. In most patients, symptoms are triggered by heat (starting at temperatures above 29°C); the remedy used is localized cooling or immersion in ice water. Trophic lesions are not associated. Generalized vasomotor dysfunction and Raynaud’s syndrome are frequently associated [1,2].
The term erythromelalgia is derived from the Greek words erythrose, meaning “red,” Melos, meaning “limb,” and algos, meaning “pain”. It was first described in 1878 by Silas Weir Mitchell and was initially called “Mitchell’s disease”. Smith and Allen proposed another term, erythermia, in 1938 to emphasize the characteristic heat of this syndrome. Two Dutch gentlemen named Drenth and Michiels proposed the name erythromelalgia in 1990 [3].
The diagnosis has been based since its discovery on the clinical features described here, with pathophysiology previously attributed to vascular, inflammatory, and/or neuropathic causes. Symptoms in fact can remain modest for years or can evolve negatively so as to lead to a functional disability, especially in forms with early-onset, typical of birth or early childhood [4].
The term “erythromelalgia” was then differentiated from “erythermia” on the basis of the response to aspirin by Drenth and Michiels, establishing the following three categories [5].
a) Erythromelalgia in thrombocythemia: It is platelet-mediated and responds to aspirin. It occurs in association with essential thrombocytosis and polycythemia vera.
b) Primary Erythermia: Refers to an idiopathic or inherited disorder. Also called aspirin-resistant erythermia of unknown origin.
c) Secondary Erythermia: Aspirin-resistant and associated with a variety of medical conditions.
The course of erythromelalgia is characterized by painful attacks (erythromelagic crisis) that last from several hours to several days. Excruciating, stabbing pain during an attack is so intense that it can drive the patient to despair. The affected limb turns red, acquires a cyanotic hue, becomes warm to the touch, and moist from sweat, in rare cases, a rash of urticaria appears. In addition, there is usually moderate swelling of the affected areas, in extensive stages, there may be necrosis. In this case, the bulb of the fingers thickens, thickens, or atrophies the skin, brittleness, and turbidity of the nails with disfigurement of the limb. Painful sensations may reduce in a horizontal position and with the application of cold, so patients try to reduce pain by removing shoes and warm clothing or lifting their legs upward. Conversely, when standing and walking, lowering one’s legs, from heavy shoes, the pain intensifies. A painful attack can be triggered by reactive hyperemia that occurs when walking, so even with early forms of the disease, patients often want to take off their shoes and walk barefoot while walking. Outside of the attack, the patient does not feel completely healthy, as the painful pain during the attack is accompanied by severe emotional disturbances. Erythromelalgia as an idiopathic form is somewhat more common in men than in women; mostly young people are sick. In rare cases, there is a type of steady-state course of the disease. The secondary syndrome of erythromelalgia is characterized by a milder course. The intensity of peripheral vascular disorders may vary from a periodic sensation of heat in the extremities with transient hyperesthesia and increased skin temperature to the development of classic erythoplasmic crises. Trophic disorders, as a rule, are not as pronounced as in the primary form of the disease. The course of the erythromelagic phenomenon, in this case, depends on the course of the underlying disease [6].
Clinical diagnosis of erythromelalgia should be based on the following symptoms: a) paroxysmal pain disorder; the nature of the pain pulses, burns, the duration of seizures from several minutes or hours to several days, interictal periods from 10-15 minutes to several weeks and more, sometimes with a steady increase in the duration of the attack; the dependence of the painful attack at the time of year, the time of day (usually in the evening, at night), the surrounding temperature, wearing warm shoes, physical stress, position of the limbs. Stimulation of pain from walking on wet sand, snow, and cold lotions with ice; b) the initial location of pain: in the first toe, sole, heel, followed by spread to the whole foot and beyond; c) symmetry of the lesion: the lower limbs are most often affected, sometimes all four limbs, rarely only the upper limbs, rarely other localizations; d) local changes: local hyperemia, sometimes with edema, hyperhidrosis; Skin coloration is most often cyanotic, maybe with cyanotic spots, sometimes marble. There are never trophic ulcers. In some cases, hyperkeratosis, and lamellar stratification of the epidermis with deep cracks are observed [7].
In the differential diagnosis of the primary and secondary forms of the disease, the following should be considered [7].
- In the secondary form: erythromelalgic crises are not as pronounced; as a rule, the history of the disease is shorter and the age of patients is older; more often there are unilateral defeats; the area of pain and injury is stationary and does not progress over time; it is possible to identify the main suffering, the treatment of which leads to a significant decrease in the manifestations of erythromelalgia.
- In the primary form: the symptoms are more acute; the age is younger, the history of the disease may be prolonged; with the passage of time, the symptomatology increases and the area of the lesion increases; more often symmetrical lesions; with the most thorough clinical examination, it is not possible to identify a disease that can cause manifestations of erythromelalgia.
The differential diagnosis includes post-traumatic reflex dystrophies, shoulder-hand syndrome, peripheral neuropathy, causalgia, Fabry disease, and bacterial cellulitis [8].
Treatment of erythromelalgia consists of avoiding exposure to heat sources, rest, limb elevation, and cold packs, and in the case of primary erythromelalgia, the administration of gabapentin, while in secondary erythromelalgia the treatment must be modulated based on the underlying pathology. Even when the primary disease with its treatment is not lost meanings in idiopathic form rhodonalgia vasoconstrictors the enamel, vitamin B12, gistaminoterapiya introduction Novocaine, assigning different species of physiotherapy (galvanic collar on Scherbakov, galvanizing zone sympathetic ganglia, alternation of hot and cold baths, bath two chambers - sulfide, radon, mud baths on segmental zones, ultraviolet irradiation paravertebral region dI, DXII), shown blo procaine nodes hells DII - DIV with the defeat of upper limbs, LI - LII - lower. Sufficiently effective is the use of acupuncture, and deep X-ray therapy on the spinal cord area. Patients should wear light shoes, and avoid overheating. In severe cases, resort to surgery (periarterial sympathectomy, preganglionic). In the idiopathic form of the disease, accompanied by a marked pain syndrome, a significant effect is produced by a stereotactic operation on the basal ganglia [8].
Since 2004, however, cases of hereditary erythromelalgia (IEM) have been linked to dominant gain-of-function mutations in the SCN9A gene and subsequent alterations in the function of the voltage-gated sodium channel Nav1.7.5. In addition, similar symptoms associated with autoimmune or myeloproliferative disorders have been reported in adults and termed “secondary erythromelalgia”, but are extremely rare in children. Thus, sodium channels (Nav1.1 through Nav1.9) have been encoded from one gene family (SCN) and are differentially distributed in the nervous system, heart, and muscles. In children, sporadic or inherited mutations affecting several voltage-conducting sodium channels have been associated with epilepsy, cardiac conduction, and skeletal muscle abnormalities, with treatment often based on nonspecific sodium channel blockers such as mexiletine. Nav1.7 channels are then expressed in peripheral nociceptive sensory neurons within the Dorsal Root Ganglia (DRG) and trigeminal ganglia, and in sympathetic ganglia neurons, and therefore play a key role in pain sensitivity. Gain-of-function mutations with IEMs typically increase the excitability of DRG neurons by hyperpolarizing the voltage-dependence of Nav1.7 channel activation (making the channels easier to activate), effectively slowing channel deactivation (which remains open longer), and consequently increasing the response to slow stimuli. It is also important to note that the site of mutation can influence both abnormalities of Nav1.7 channel function and age of onset and severity of symptoms, and while reports in adults have assessed phenotype-genotype relationships, details of clinical evaluation during childhood and/or genetic testing results have not been available in all pediatric case series [8].
Methods
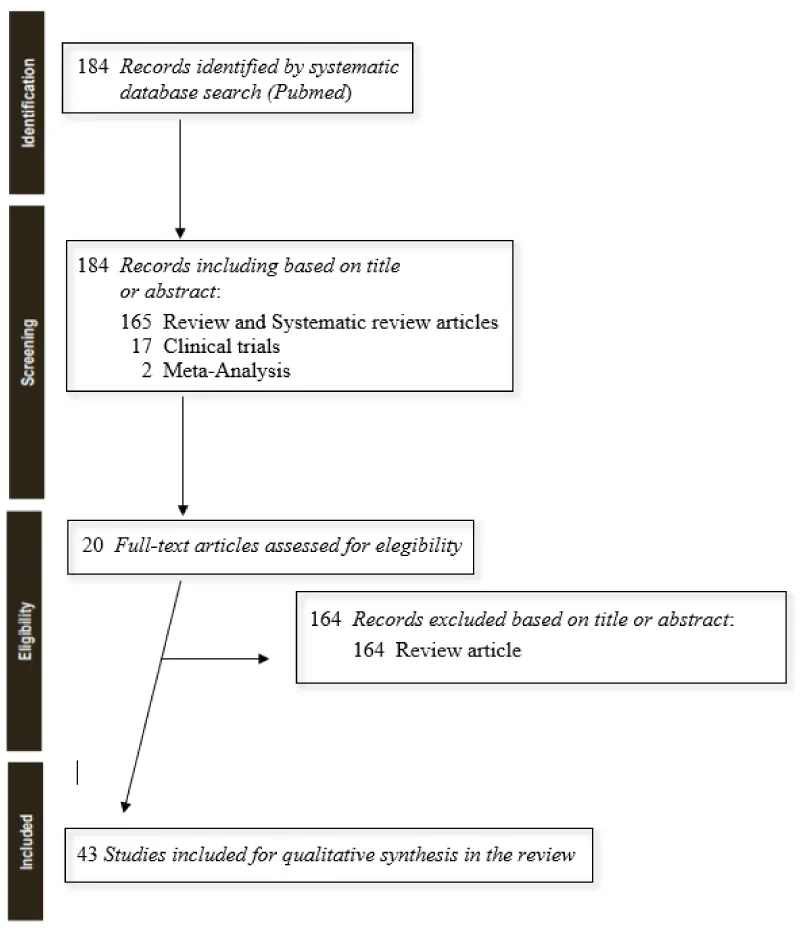
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [9]. To identify the reported symptoms, management, and complications of SCN9A-positive IEM in Children and Youth (CYP), we searched PubMed (January 2019 to December 2021) using the search term “erythromelalgia” (which also identified “erythermia”), as a systematic review had already been published in March 2019 that examined all profiles of clinical interest [1].
The search, thus structured, revealed the presence of 19 manuscripts, including a clinical trial, meta-analysis, and randomized controlled trial and excluding reviews, systematic reviews, books, and documents, for the purpose of the clinical update.
The present work aims at the one hand to enrich that work by adding recent data from the last 3 years and on the other hand to present a single case that presents special characteristics. No additional eligible publications were found from the search in PsycINFO, EMBASE, or Cochrane databases. Records were screened and limited to those published in English. Citations deemed relevant and inclusive of the criteria were screened full-text.
Literature update
The state of the art through 2019 captured a total of twenty-eight publications describing erythromelalgia associated with 15 different SCN9A gene variants in 25 children. The pain was severe and often refractory to multiple treatments, including nonspecific sodium channel blockers. Skin damage or other complications of cold immersion for symptomatic relief were common (60%). SCN9A mutations that resulted in increased hyperpolarizing shifts in Nav1.7 sodium channels were related to symptom onset at younger ages. Variability in reporting and potential publication bias toward severe cases limited any estimate of overall prevalence, and in this research, symptoms were similar but comorbidities were more common in children with SCN9A mutations; quantitative sensory testing also revealed marked dynamic warm allodynia. It concluded that: “Inherited erythromelalgia in children is associated with difficult-to-manage pain and significant morbidity. Standardized reporting of outcome and management in larger series will strengthen the identification of genotype-phenotype relationships. More effective long-term therapies are a significant unmet clinical need” [1]. However, another study from 1999 that suggested the use of Pramipexol [10] for erythromelalgia as well was not considered in this research. It is a novel non-ergot dopamine agonist that has high selectivity for interaction with dopamine D2 receptors (especially the D3 receptor subtype). It has been effective in early Parkinson’s disease as monotherapy and as adjunctive therapy with L-dopa in advanced stages of the disease. Clinical improvement can be observed after 3 to 4 weeks of treatment. The adverse event profile of pramipexole is similar, in general, to that of other dopamine receptor agonists, although it can be expected that pramipexole should not induce side effects related to the chemical structure of ergot, such as erythromelalgia, distal vasospasm, retroperitoneal fibrosis, or pleural effusions. However, the study concludes, that the potential benefits of this promising dopamine agonist should be tested in well-designed prospective comparative studies with other ergot dopamine agonists and not;In the following years, several studies have focused on the use of this molecule on diseases such as Parkinson’s [11], fibromyalgia [12], bipolar depression [13], restless legs syndrome [14], Tourette’s syndrome [15], sleep disorders [16,17] and several other neurodegenerative conditions [18], but not erythromelalgia.
Subsequent research over the last three years has revealed the following
- Erythromelalgia must be distinguished from red ear syndrome (or auricular erythromelalgia). In the scientific literature, a little more than one hundred cases are described to date in about 102 patients, with an average age of onset around the fourth decade of age. The syndrome is classified in the group of trigeminal autonomic headaches (TAC)s, with which it can coexist or be secondary. The syndrome is closely related to episodes of primary headache; moreover, the red ear is characteristic of migraine in pediatric patients, similar to osmophobia and allodynia. Its origin is unknown; an association with spondylolisthesis in C2-C3 is often observed; it is also associated with Costen’s syndrome, glossopharyngeal nerve neuralgia, or migraine. This syndrome pathogenically appears to be attributable to antidromic sense release of vasodilator peptides from afferent nerve terminals in response to irritation of the C3 nerve root. The syndrome causes crises of severe burning pain of the abscess type with heat to one or both auricles, the ear appearing reddened and warm. Symptomatology is often triggered by chewing or mechanical contact manipulations such as straining, heat or cold, stress, neck movements, and hair washing or brushing. Symptoms may also manifest with hyperacusis, intermittent tinnitus, and subjective hearing difficulties. The duration of seizures is seconds or hours, while the frequency can vary from several times a day to a few episodes per year. Drugs commonly used to treat the syndrome include gabapentin (common with erythromelalgia), amitriptyline, propranolol, flunarizine, nonsteroidal anti-inflammatory drugs, and analgesic blockade of the same side of the C2-C3 nerve root; methysergide or application of a cold compress and imipramine have also been shown to be useful [19].
- Erythromelalgia must be distinguished from red scrotum syndrome. The skin of the genitals can be affected by a variety of dermatoses, whether inflammatory, infectious, malignant, idiopathic, or others. Red scrotum syndrome is characterized by persistent erythema of the scrotum associated with a burning sensation, hyperalgesia, and itching. Its cause is unknown, but proposed mechanisms include rebound vasodilation after prolonged use of topical corticosteroids and localized erythromelalgia; for this reason, the clinical boundaries of this condition are unclear. However, the condition is chronic, and treatment is often difficult [20].
- SCN9A neuropathic pain syndromes (SCN9A-NPS) include SCN9A erythromelalgia (EM), SCN9A paroxysmal extreme pain disorder (PEPD), and SCN9A small fiber neuropathy (SFN). SCN9A-EM is characterized by recurrent episodes of intense bilateral burning pain, redness, heat, and occasional swelling. While the feet are more commonly affected than the hands, the legs, arms, face, and/or ears may be involved in severely affected individuals. SCN9A-PEPD is characterized by neonatal or infantile-onset of autonomic manifestations that may include skin redness, harlequin color change (mottled or asymmetric), and non-epileptic tonic seizures (stiffening), and syncope with bradycardia. Later manifestations are episodes of burning deep rectal, ocular, or submandibular pain accompanied by redness (erythematous skin changes). SCN9A-SFN is characterized by neuropathic pain in adulthood with sock and glove distribution, often with a burning quality; autonomic manifestations such as dryness of the eyes, mouth, orthostatic dizziness, palpitations, bowel or bladder disorders; and preservation of large nerve fiber function (normal strength, tendon reflexes, and vibration sense). The diagnosis of SCN9A-NPS is established in a proband with a heterozygous pathogenic variant in SCN9A identified by molecular genetic testing. Triggers include heat, standing, alcohol, and spicy foods (SCN9A-EM); defecation, cold wind, eating, and emotions (SCN9A-PEPD); and diabetes mellitus, alcohol, and chemotherapy (SCN9A SFN). Most affected individuals are treated in dermatology, neurology, or pain clinics, or by anesthesiologists who specialize in chronic pain management: 1) SCN9A-EM. Cooling the extremities reduces pain; note that the use of a ventilator is preferable to prolonged immersion in cold water, which can result in skin maceration, infection, and gangrene. Medications to consider are nonselective sodium channel blockers (eg, carbamazepine, lidocaine infusion, or oral mexiletine). 2) SCN9A-PEPD. Use of stool softeners and slow stool passage to reduce the likelihood of triggering an attack. Carbamazepine is the most effective treatment (although not entirely) in reducing the number and severity of seizures. Other anti-seizure medications with variable efficacy include lamotrigine, topiramate, tiagabine, and sodium valproate. 3) SCN9A-SFN. Lacosamide is associated with reduced pain ratings, improved general well-being, and improved sleep quality, but no change in overall quality of life or autonomic manifestations. SCN9A neuropathic pain syndromes are inherited in an autosomal dominant manner. Each child of an individual with a variant causing NPS in SCN9A has a 50% chance of inheriting the variant. Once the pathogenic SCN9A variant has been identified in an affected family member, prenatal testing for an increased risk pregnancy and preimplantation genetic testing are possible [21].
- The use of spinal cord stimulation has been described in multiple cases with success reported for up to 24 months. However, the use of dorsal root ganglion (DRG) stimulation for erythromelalgia-related pain has not been described, except in the following study presenting a case of erythromelalgia-related pain on the bilateral plantar surfaces of the feet, successfully treated with DRG stimulation of the bilateral S1 sacral nerve root [22].
- The causes of neuropathic pain are multiple and remain unexplained in most cases. Alterations in the electrical excitability of nociceptive neurons by pathogenic mutations in sodium channels lead to disease patterns such as small fiber neuropathy and various pain syndromes. Therefore, treatment of patients with chronic neuropathic pain requires interdisciplinary cooperation and is often difficult because of unsatisfactory responses to treatment. Increased knowledge about rare genetically determined channelopathies may contribute to the development of new drugs because ion channels are central players in pain processing [23].
- Vixotrigine is a voltage- and use-dependent sodium channel blocker currently in development for the treatment of various neuropathic pain indications. In one study, with a total of 10,263 pharmacokinetic samples collected from 465 included subjects, it was found that the pharmacokinetics of vixotrigine were adequately described by a two-compartment model with two compartments of first-order transit absorption and elimination [24].
- Nonspecific reactions at the injection site of anticovid vaccine that occur very early are the most common. Type I hypersensitivity reactions (e.g., urticaria, angioedema, and anaphylaxis) probably due to ingredient allergy may occur rarely but may be severe. Type IV hypersensitivity reactions may be observed, including large delayed local skin lesions (“COVID arm”), inflammatory reactions at sites of dermal fillers or previous radiation or even old BCG scars, and most commonly morbilliform eruptions and erythema multiforme-like. Autoimmune-mediated skin findings after COVID-19 vaccination include leukocytoclastic vasculitis, lupus erythematosus, and immune thrombocytopenia. Functional angiopathy (chilblain-like lesions, erythromelalgia) may also be observed. Pityriasis rosea-like skin eruptions and reactivation of herpes zoster have also been reported after COVID-19 vaccination [25].
Aetiopathogenesis
Thus, if the second form is well identified as a consequence of a primary disorder to be identified and corrected, the primary (or idiopathic) form still remains a clinical mystery. Many hypotheses are at stake [1,2].
A possible cause of the disease was considered peripheral neuritis, in relation to which in some patients by resection of peripheral nerves the impulses from the affected nerve endings were eliminated. The similarity of erythromelagic phenomenon was observed in patients with middle nerve damage [4].
In contrast, however, to the view of the peripheral origin of the disease, Degio believed that this disease had a central medullary origin. A similar view was shared by other researchers. According to their ideas, at the heart of erythromelalgia is the change in the gray matter of the lateral and posterior horns of the spinal cord, accompanied by paralysis of vasomotor fibers. This has been confirmed by observations on the development of erythromelagic syndrome in patients with various spinal cord injuries [5].
The phenomenon of rhodonalgia then is explained by the injury of the centers of the diencephalic regions (thalamic and subthalamic XYZ) around ventricle III, based on the monitoring of patients with pathology of the relevant areas of the brain [6].
At the same time, the connection between the manifestations of erythromelalgia and Raynaud’s disease is emphasized. These hypotheses are confirmed by observations on the positive outcome of the erythromelagic phenomenon, which developed in the framework of the third phase of the Reino phenomenon, which arose after sympathectomy [7].
Denying the role of the nervous system in erythromelalgia, some authors have considered the cause of the disease in the various changes in the arterial wall. Thus, a combination of erythromelalgia with Osler-Randu disease (hereditary hemorrhagic telangiectasia) is described. There is evidence that other diseases with primary vascular wall injury often lead to erythromelalgic attacks. Cases of erythromelalgia combined with polycythemia (Vakez disease) are still described [26].
There is a view that erythromelalgia is vasomotor neurosis and can occur in people with mental features. The development of erythromelalgia in children with psychosis has been observed. There were also some humoral aspects of the theory of the pathogenesis of erythromelalgia. The onset of the disease is associated with a violation of serotonin metabolism, as indicated by the relief of patients after taking reserpine and the appearance of the erythromelagic syndrome in serotonin-producing tumors [27].
But the real discovery was the correlation with the SCN9A gene. The SCN9A gene belongs to a family of genes that provide instructions for making sodium channels. These channels, which transport positively charged sodium atoms (sodium ions) into cells, play a key role in a cell’s ability to generate and transmit electrical signals. The SCN9A gene provides instructions for making one part (the alpha subunit) of a sodium channel called NaV1.7. NaV1.7 sodium channels are found in nerve cells called nociceptors that transmit pain signals. Nociceptors are part of the peripheral nervous system, which connects the brain and spinal cord to cells that detect sensations such as touch, smell, and pain. Nociceptors are primarily involved in transmitting pain signals. The centers of nociceptors, known as the cell bodies, are located in a part of the spinal cord called the dorsal root ganglion. Fibers called axons extend from the cell bodies, reaching throughout the body to receive sensory information. Axons transmit the information back to the dorsal root ganglion, which then sends it to the brain. NaV1.7 sodium channels are also found in olfactory sensory neurons, which are nerve cells in the nasal cavity that transmit smell-related signals to the brain. Several are the pathologies related to mutations of this gene; among the most important we find the congenital pain insensitivity syndrome, the extreme pain disorder paroxysmal, the small fiber neuropathy, genetic epilepsy with high fever, the type II autosomal hereditary sensory neuropathy, and finally the erythromelalgia itself. More than 10 mutations in the SCN9A gene have been found to cause erythromelalgia, a condition characterized by episodes of pain, redness, and swelling in various parts of the body, particularly the hands and feet. All identified mutations change one protein building block (amino acid) in the NaV1.7 sodium channel. These mutations result in a NaV1.7 sodium channel that opens more easily than usual and stays open longer than normal, increasing the flow of sodium ions that produce nerve impulses within nociceptors. This increase in sodium ions enhances the transmission of pain signals, leading to the signs and symptoms of erythromelalgia. However, an estimated 15% of cases of erythromelalgia are caused by mutations in the SCN9A gene. Other cases are thought to have a nongenetic cause or may be caused by mutations in one or more as-yet-unidentified genes or being confirmed with a more representative statistical sample [28-43].
Single case
A.A., the male, was born in 2008, to non-consanguineous parents. A.’s clinical history begins with the symptomatic manifestation of restlessness and pain, in the first summer month at only 8 months and a half; symptoms regressed once he returned from his summer vacation in a cooler place. Symptoms seemed to disappear until the following summer when he began to suffer from localized pain, intense heat, and itching; symptoms again disappeared after returning from the vacation. Typical pediatric diseases were excluded. In the summer of 2011, the patient began to experience severe malaise, consisting of continuous crying, as if he had been struck by sunstroke; all symptoms that regressed by using fans and cold air conditioners. In the summer of 2012, the symptoms became more acute, and only compresses with ice and water from the refrigerator were able to alleviate, to the point that further medical checks focused on allergy and autoimmune profiles. It was only in those months that the diagnosis of erythromelalgia arrived for the first time, although in the absence of complete serum and genetic investigations, and the assumption of paracetamol, codeine, acetylsalicylic acid, and ketoprofen helped to reduce but not to make disappear the symptomatology suffered; useless the attempts to find remedy in oriental and Chinese medicine (acupuncture and local applications of Wang Bu Liu Xin seeds). Myalgic crises become more and more intense and unbearable, often lasting more than two weeks: “during the crises, A. does not sleep because his body burns so much that he tries to rest but is awakened by the pains, so the problem is not only his pathology that involves a danger for the high body temperature and the damage it can cause to the organs but the risk that the lack of sleep can bring to the heart brain”. In these cases, only morphine could provide relief and extinguish these symptoms. In 2016, after several attempts also with non-traditional medicines, the young patient uses prescription mexiletine, an antiarrhythmic for the treatment of dystrophic and non-dystrophic myotonia and alterations of the function of the chlorine or sodium channel, with excellent general benefits. Currently, the clinical picture is not yet stable because the drug therapy followed and prescribed (mexiletine 150mg for 2/days, ketotifen 20mg for 1/day only for the spring-summer period, indomethacin 50 mg for 1 day only for migraines, cannabidiol 5 drops for 2/days, carbamazepine 200mg for 2 / day, in addition to supplements of vitamin C, D, omega 3, multivitamins and probiotics such as lactobacillus, bifidobacteria e Streptococcus thermophilus) does not prevent the onset of symptoms, although the situation is more under control. The investigations carried out show a picture of microcytosis, low lymphocytes, anemia, and hypochromia, beyond a pediatric reference of slow growth and significant thinness (13y, 156cm/36kg), however compatible for symptomatology to the “idiopathic erythromelalgia on the genetic basis”, although in the absence of positivity to the genetic investigation on the gene SCN3A, 9A, 10A and 11A, Fabry disease and mutations in NALP3 and NALP12.
Conclusion
Although clinical publications on this morbid condition report as many as 16 different Nav1 channel substitutions 7 and more than 40 pharmacological treatments including agents with predominant but not specific sodium channel blocking activity (mexiletine, lidocaine, carbamazepine), anti-neuropathic drugs (gabapentinoids and antidepressants), antidepressant drugs with efficacy on migraines (amitriptyline), vasoactive drugs for the management of hypertension and analgesics (opioids and ketamine) [1], current research suggests new genetic hypotheses yet to be tested and the central importance of genetic counseling, to inform patients and their families about severity, likely course of symptoms, and risk of complications, and in some cases to guide clinical management. Current findings and the significant morbidity associated with the condition, including in light of the single case presented, highlight the need for mechanism-based therapies to improve clinical outcomes.
- Arthur L, Keen K, Verriotis M, Peters J, Kelly A, et al. (2019) Pediatric erythromelalgia and SCN9Amutations: systematic review and single-center case. J Pediatr 206: 217-224.e9. Link: https://bit.ly/3uxMOYG
- Jka SK, Karna B, Goodman MB (2021) Erythromelalgia. In StatPearls. Treasure Island (FL): StatPearls Publishing. PMID: 32491719. Link: https://bit.ly/3JrTjk9
- Drenth JP, Michiels JJ (1994) Erythromelalgia and erythermalgia: diagnostic differentiation. Int J Dermatol 33: 393-397. Link: https://bit.ly/3rky79h
- Saliba AN, Taher AT, Besa EC, Nardino RJ, Silber ALM, et al. (2020) Erythromelalgia. Medscape. Drugs & Disease. Emedicine.medscape. Link: https://bit.ly/3E89JNA
- Kuhnert SM, Phillips J, Davis MDP (1999) Lidocaine and Mexiletine Therapy for Erythromelalgia. Arch Dermatol 135: 1447-1449. Link: https://bit.ly/3E4xciy
- Layzer RB (2001) Hot feet: erythromelalgia and related disorders. J Child Neurol 16: 199-202. Link: https://bit.ly/3uvh5aG .
- Jorgensen HP, Sondergaard J (1978) Pathogenesis of erythromelalgia. Arch Dermatol 114: 112-114. Link: https://bit.ly/3uuE8SX
- Leroux MB (2018) Erythromelalgia: a cutaneous manifestation of neuropathy? An Bras Dermatol 93: 86-94. Link: https://bit.ly/38yuztw
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097. Link: https://bit.ly/367aHNq
- Grandas F, Galiano ML (1999) Pramipexol: a new dopaminergic agonist for the treatment of Parkinson disease. Neurologia 14: 224-228. Link: https://bit.ly/38L1qeT .
- Cacabelos R (2017) Parkinson's Disease: From Pathogenesis to Pharmacogenomics. Int J Mol Sci 18: 551. Link: https://bit.ly/3vdz9VI
- Sumptn JE, Moulin DE (2014) Fibromyalgia. Handb Clin Neurol 119: 513-527. Link: https://bit.ly/37FyjJb
- Shen YC (2018) Treatment of acute bipolar depression. Ci Ji Yi Xue Za Zhi 30: 141-147. Link: https://bit.ly/3xkBL6R
- Winkelmann J, Allen RP, Högl B, Inoue Y, Oertel W, et al. (2018) Treatment of restless legs syndrome: Evidence-based review and implications for clinical practice. Mov Disord 33: 1077-1091. Link: https://bit.ly/3M0Ky2e
- Quezada J, Coffman KA (2018) Current Approaches and New Developments in the Pharmacological Management of Tourette Syndrome. CNS Drugs 32: 33-45. Link: https://bit.ly/3uwNZrl
- Jung Y, St Louis EK (2016) Treatment of REM Sleep Behavior Disorder. Curr Treat Options Neurol 18: 50. Link: https://bit.ly/3utC0Lc
- Perrotta G (2019) Sleep-wake disorders: Definition, contexts and neural correlations. J Neurol Psychol 7: 09. Link: https://bit.ly/3v9RS4v
- Jiang H, Huang J, Shen Y, Guo S, Wang L, et al. (2017) RBD and Neurodegenerative Diseases. Mol Neurobiol 54: 2997-3006. Link: https://bit.ly/3vaTxXD
- Cinats AK, Haber RM (2019) Pediatric red ear syndrome: A Review Article of an erythromelalgia type and review of the literature. Pediatric Dermatol 36: 686-689. Link: https://bit.ly/3rixlK8
- Khalil S, Kurban M, Abbas O (2020) Red scrotum syndrome: An update on clinicopathologic features, pathogenesis, diagnosis, and management. J Am Acad Dermatol S0190-9622(20)30988-9. Link: https://bit.ly/3LXqHAR
- Hisama FM, Dib-Hajj SD, Waxman SG, Adam MP, Ardinger HH, et al. (2020) SCN9A Neuropathic Pain Syndromes. In GeneReviews. Seattle (WA): University of Washington, Seattle. PMID: 20301342. Link: https://bit.ly/3xltsb5
- Hagedorn JM, Canzanello N, Lamer TJ (2021) Dorsal Root Ganglion Stimulation for Erythromelalgia Related Foot Pain: A Review Article and Review of the Literature. Pain Pract 21: 698-702. Link: https://bit.ly/3juhwvx
- Dohrn MF, Lampert A, Üçeyler N, Kurth I (2019) Neuropathic pain syndromes and channelopathies. Internist (Berl) 60: 90-97. Link: https://bit.ly/3JroJXO
- Naik H, Zhao Y, Forrestal F, Cleall S, Bockbrader H, et al. (2021) Population Pharmacokinetics of Vixotrigine in Healthy Volunteers and Subjects with Trigeminal Neuralgia, Painful Lumbosacral Radiculopathy and Erythromelalgia. Eur J Drug Metab Pharmacokinet 46: 395-404. Link: https://bit.ly/3uxdCYZ
- Gambichler T, Boms S, Susok L, Dickel H, Finis C, et al. (2021) Cutaneous findings following COVID-19 vaccination: review of world literature and own experience. J Eur Acad Dermatol Venereo 36: 172-180. Link: https://bit.ly/3O7PILp
- SCN9A gene. Medlineplus.
- Cox JJ, Nicholas AK, Thornton G, Roberts E, Springell K, et al. (2006) An SCN9A channelopathy causes congenital inability to experience pain. Nature 444: 894-898. Link: https://bit.ly/3xkOMxi
- Dib-Hajj SD, Cummins TR, Black JA, Waxman SG (2007) From genes to pain: Na v 1.7 and human pain disorders. Trends Neurosci 30: 555-563. Link: https://bit.ly/3vezW8U .
- Dib-Hajj SD, Yang Y, Waxman SG (2008) Genetics and molecular pathophysiology of Na(v)1.7-related pain syndromes. Adv Genet 63: 85-110. Link: https://bit.ly/3riKRx4
- Doty CN (2010) SCN9A: another sodium channel excited to play a role in human epilepsies. Clin Genet 77: 326-328. Link: https://bit.ly/3O0Kq4q
- Drenth JP, Waxman SG (2007) Mutations in sodium-channel gene SCN9A cause a spectrum of human genetic pain disorders. J Clin Invest 117: 3603-3609. Link: https://bit.ly/38KCIeE
- Faber CG, Hoeijmakers JG, Ahn HS, Cheng X, Han C, et al. (2012) Gain of function Naν1.7 mutations in idiopathic small fiber neuropathy. Ann Neurol 71: 26-39. Link: https://bit.ly/3KynvLR
- Fertleman CR, Ferrie CD, Aicardi J, Bednarek NA, Eeg-Olofsson O, et al (2007) Paroxysmal extreme pain disorder (previously familial rectal pain syndrome). Neurology 69: 586-595. Link: https://bit.ly/3JrTKeh
- Fischer TZ, Waxman SG (2010) Familial pain syndromes from mutations of the NaV1.7 sodium channel. Ann N Y Acad Sci 1184: 196-207. Link: https://bit.ly/3LVITKZ
- Goldberg YP, MacFarlane J, MacDonald ML, Thompson J, Dube MP, et al. (2007) Loss-of-function mutations in the Nav1.7 gene underlie congenital indifference to pain in multiple human populations. Clin Genet 71: 311-319. Link: https://bit.ly/376qUmD
- Hoeijmakers JG, Merkies IS, Gerrits MM, Waxman SG, Faber CG, et al. (2012) Genetic aspects of sodium channelopathy in small fiber neuropathy. Clin Genet 82: 351-358. Link: https://bit.ly/3rg8A1e
- Houlden H (2012) Extending the clinical spectrum of pain channelopathies. Brain 135: 313-316. Link: https://bit.ly/3E3TbpK
- Lampert A, O'Reilly AO, Reeh P, Leffler A (2010) Sodium channelopathies and pain. Pflugers Arch 460: 249-263. Link: https://bit.ly/3O655E8
- Meisler MH, O’Brien JE, Sharkey LM (2010) Sodium channel gene family: epilepsy mutations, gene interactions and modifier effects. J Physiol 588: 1841-1848. Link: https://bit.ly/38L3rI3
- Singh NA, Pappas C, Dahle EJ, Claes LR, Pruess TH, et al. (2009) A role of SCN9A in human epilepsies, as a cause of febrile seizures and as a potential modifier of Dravet syndrome. PLoS Genet 5: e1000649. Link: https://bit.ly/3O6Qs3C
- Waxman SG (2006) Neurobiology: a channel sets the gain on pain. Nature 444: 831-832. Link: https://bit.ly/3xlrLuk
- Waxman SG (2011) Neuroscience: Channelopathies have many faces. Nature 472: 173-174. Link: https://bit.ly/3uzlcma
- Young FB (2007) When adaptive processes go awry: gain-of-function in SCN9A. Clin Genet 73: 34-36. Link: https://bit.ly/3KyoI5R
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
