Global Journal of Infectious Diseases and Clinical Research
Acute Inflammatory Demyelinating Polyneuropathy Following Japanese Encephalitis: A Rare Neurological Sequela
1SR – DM Clinical Infectious Diseases, AIIMS Raipur, India
2HoD Medicine, AIIMS Raipur, India
3Associate Professor, Medicine, AIIMS Raipur, India
Author and article information
Cite this as
Mishra AB, Pandit V, Kannauje P. Acute Inflammatory Demyelinating Polyneuropathy Following Japanese Encephalitis: A Rare Neurological Sequela. Glob J Infect Dis Clin Res. 2025; 11(1): 010-012. Available from: 10.17352/2455-5363.000064
Copyright License
© 2025 Mishra AB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Japanese Encephalitis (JE) is a neurotropic viral infection endemic to Asia, primarily transmitted by Culex mosquitoes. While Central Nervous System (CNS) involvement is well-documented, peripheral nervous system complications such as Acute Inflammatory Demyelinating Polyneuropathy (AIDP)—a variant of Guillain-Barré Syndrome (GBS)—remain exceedingly rare. We report the case of a 20-year-old male presenting with altered sensorium, seizures, and progressive limb weakness. Neuroimaging revealed meningoencephalitis with an acute infarct in the left parietal region. Japanese Encephalitis Virus (JEV) IgM antibodies were detected in Cerebrospinal Fluid (CSF), confirming the diagnosis. The patient subsequently developed respiratory failure and flaccid quadriparesis. Nerve conduction studies showed demyelinating sensorimotor polyradiculoneuropathy, consistent with AIDP. Despite immunotherapy with Intravenous Immunoglobulin (IVIg), neurological recovery was minimal, and the patient remained ventilator-dependent. This case underscores the need for heightened clinical vigilance for atypical peripheral neuropathies in JE patients, as early diagnosis and intervention may alter outcomes.
Japanese Encephalitis (JE), caused by the Japanese Encephalitis Virus (JEV), remains a leading cause of viral encephalitis in Asia, with an estimated 68,000 cases annually [1]. Transmitted primarily through Culex mosquitoes, JEV is maintained in zoonotic cycles involving pigs and waterfowl. Although most JEV infections are asymptomatic, symptomatic cases may present with fever, altered mental status, and seizures, often progressing to coma or death in severe cases [2].
Neurological complications of JE are typically confined to the Central Nervous System (CNS), including encephalitis, movement disorders, and seizures. However, rare associations with Peripheral Nervous System (PNS) pathologies, such as Guillain-Barré Syndrome (GBS), have been described [3]. AIDP, the most common GBS variant, involves immune-mediated demyelination of peripheral nerves and can result in life-threatening respiratory failure if not promptly recognized and managed [4].
The exact pathophysiological link between JEV and AIDP remains poorly understood, though molecular mimicry and immune dysregulation are suspected mechanisms. A few case series suggest that only 2% - 4% of JE patients develop AIDP [5,6], making such presentations both rare and diagnostically challenging.
This case report aims to contribute to the limited literature on JE-associated AIDP by presenting a severe clinical course in a young adult male, emphasizing the importance of early recognition of peripheral neurological involvement in the context of JE.
Case presentation
A 20-year-old previously healthy male presented on November 24 with a two-day history of high-grade fever and dyspnea, followed by headache, vomiting, and progressive right-sided limb weakness. On the day of admission, he experienced a generalized tonic-clonic seizure with ocular deviation and subsequently developed altered sensorium.
Initial examination revealed a Glasgow Coma Scale (GCS) score of E2V2M3, later deteriorating to E1VtM1. Vital signs included heart rate 90/min, BP 102/46 mmHg, respiratory rate 35/min, SpO₂ 65% on room air, and a core temperature of 104 °F. Pupils were pinpoint and sluggishly reactive. Neurological exam showed flaccid quadriparesis—right-sided (1/5) more affected than the left (3/5)—with absent deep tendon reflexes and bilaterally mute plantar responses.
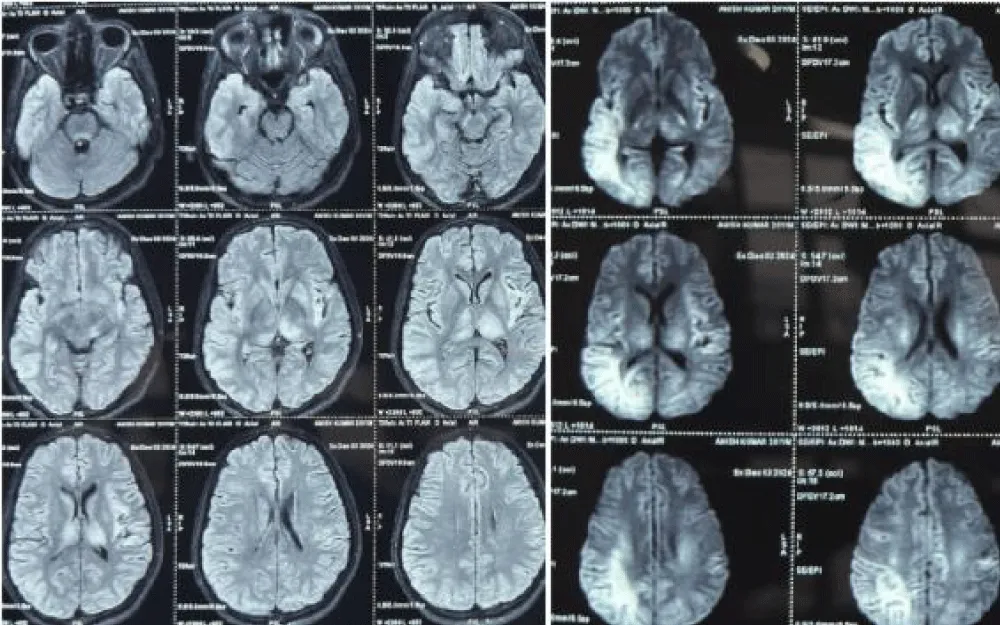
An urgent MRI brain showed non-restricted diffusion in the left thalamus, left insula, and left median parietal cortex with meningeal enhancement and an acute infarct, consistent with viral meningoencephalitis. Initial laboratory investigations, including serology for leptospira, scrub typhus, and malaria, were negative. EEG revealed intermittent theta activity with generalized slowing. CSF analysis showed two WBCs (100% lymphocytes), glucose of 68 mg/dL, and protein of 47 mg/dL. CSF viral PCR was negative, but JEV-specific IgM antibodies were detected, confirming Japanese encephalitis.
Supportive management with IV antibiotics, antivirals, anti-edema agents, and antiepileptics was initiated. On day three of hospitalization, the patient developed hypercapnic respiratory failure, necessitating intubation and mechanical ventilation. Around day seven, he developed Ventilator-Associated Pneumonia (VAP), confirmed by clinical and microbiological parameters (fever, leukocytosis, new infiltrates, and growth of Klebsiella pneumoniae sensitive to meropenem). He required one episode of cardiopulmonary resuscitation due to sudden bradycardia and was successfully revived after 2 minutes of CPR.
Persistent flaccid quadriparesis and areflexia prompted Nerve Conduction Studies (NCS) on day 10, revealing prolonged distal latencies and reduced conduction velocities in both motor and sensory nerves, consistent with demyelinating sensorimotor polyradiculoneuropathy. Repeat CSF showed albuminocytologic dissociation. A diagnosis of JE-associated AIDP was made. Intravenous immunoglobulin (IVIg) therapy was initiated at 0.4 g/kg/day for 5 days starting on day 11 post-admission.
Despite immunotherapy, improvement was minimal. The patient showed some recovery in intrinsic foot muscle strength and was able to visually track moving objects, but remained ventilator-dependent. He was transferred to a high-dependency unit for long-term care (Figure 1).
Discussion
Japanese encephalitis is known for its predilection for the CNS, particularly involving the thalami, basal ganglia, and brainstem. Neuroimaging in this patient revealed hallmark findings of JE, including thalamic and parietal lobe involvement. However, the subsequent emergence of symmetric flaccid paralysis, areflexia, and respiratory failure raised suspicion for concurrent peripheral nerve involvement.
Differential diagnoses considered included other variants of GBS, such as Acute Motor Axonal Neuropathy (AMAN) and Acute Motor-Sensory Axonal Neuropathy (AMSAN). However, electrophysiological features—including prolonged latencies, slowed conduction velocities, and temporal dispersion—favored AIDP, the demyelinating form. Albuminocytologic dissociation further supported this diagnosis.
The pathogenesis linking JE and AIDP remains unclear but is likely to involve post-infectious immune mechanisms. Molecular mimicry between viral antigens and peripheral nerve components may induce an aberrant immune response, leading to demyelination [4]. In our case, the delayed onset of peripheral symptoms and CSF profile support this immune-mediated mechanism.
What makes this case particularly unique is the rapid CNS deterioration coupled with a rare peripheral demyelinating process in a young adult with no prior comorbidities. Furthermore, the patient’s poor response to IVIg could be attributed to the delay in diagnosis of AIDP, the severity of encephalitic involvement, and the presence of systemic complications such as VAP and cardiopulmonary instability. Early administration of IVIg, ideally within the first few days of symptom onset, is critical in AIDP to prevent irreversible nerve damage [7].
Few case reports or series have highlighted the coexistence of JE with GBS. One Indian series documented AIDP in 2 out of 12 JE patients presenting with limb weakness [5]. However, comprehensive clinical details are sparse, and there is a paucity of data regarding treatment outcomes, emphasizing the value of this report.
Conclusion
This case highlights a rare but clinically significant complication of Japanese encephalitis—Acute Inflammatory Demyelinating Polyneuropathy (AIDP). Clinicians should consider the possibility of peripheral nervous system involvement in JE patients exhibiting progressive flaccid weakness or respiratory compromise. Timely recognition and prompt initiation of immunotherapy, such as IVIg, are crucial to mitigate long-term disability. This report underscores the importance of comprehensive neurological assessment in JE and calls for greater awareness of overlapping CNS and PNS manifestations.
- World Health Organization. Japanese Encephalitis [Internet]. 2023 [cited 2025 Jun 14]. Available from: https://www.who.int/news-room/fact-sheets/detail/japanese-encephalitis
- Solomon T, Dung NM, Kneen R, Gainsborough M, Vaughn DW, Khanh VT. Neurological manifestations of Japanese encephalitis. Lancet. 2000;355(9209):1056–9. Available from: https://doi.org/10.1136/jnnp.68.4.405
- Arafat SM, Zhang YH, Tan ZR, Huang J, Zhao YW. Guillain-Barré syndrome following Japanese encephalitis: a case report. J Neurol Sci. 2006;244(1-2):81–4. Available from: https://doi.org/10.1089/vim.2014.0049
- Yuki N, Hartung HP. Guillain–Barré syndrome. N Engl J Med. 2012;366(24):2294–304. Available from: https://doi.org/10.1056/nejmra1114525
- Misra UK, Kalita J, Agarwal A. A study of Japanese encephalitis and other viral encephalitis in Uttar Pradesh, India. Postgrad Med J. 2000;76(891):579–82.
- Chaudhuri A, Kennedy PGE. Guillain–Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol. 2008;4(9):478–86.
- Hughes RAC, Swan AV, Raphael JC, Annane D, van Koningsveld R. Immunotherapy for Guillain–Barré syndrome: a systematic review. Brain. 2007;130(9):2245–57. Available from: https://doi.org/10.1093/brain/awm004
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
