Archive of Gerontology and Geriatrics Research
Temporomandibular Joint Arthritis Resembling Bifid Condyle - A CBCT Analysis of 2 Cases
S Jayachandran, Priyanka Khobre* and K Sarala
Cite this as
ayachandran S, Khobre P, Sarala K (2016) Temporomandibular Joint Arthritis Resembling Bifid Condyle - A CBCT Analysis of 2 Cases. Peertechz J Gerontol Geriatr Res 1(1): 003-005. DOI: 10.17352/aggr.000002Rheumatoid arthritis is an autoimmune disorder which can cause temporomandibular joint involvement with clinical symptoms such as pain, swelling, crepitation and movement impairment. Surface erosion is one of the radiologic feature of rheumatoid arthritis and if it is involving carter of the condylar surface, it can be misdiagnosed for the bifid condyle. Here we report two cases of rheumatoid arthritis with temporomandibular joint involvement where cone beam computed tomography appearance is mimicking bifid condyle because of erosion of the condylar surface.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory condition characterized by synovial inflammation, autoantibody production (anti–citrullinated protein antibody and rheumatoid factor) and systemic features including pulmonary, psychological, cardiovascular and skeletal disorders. It mainly affects the periarticular tissue such as synovial membrane, cartilage, joint capsule, tendon, ligaments and articular bone [1,2]. Rheumatoid arthritis has prevalence of 2- 2.5% in general population with female predilection [1]. Clinically, 4-80% of RA patients show temporomandibular joint (TMJ) involvement such as pain, swelling, crepitation and movement impairment. In RA patient, diagnosis of TMJ involvement is based on history, clinical findings, radiologic features and laboratory values [3]. Although, its etiology remains unclear, according to twin studies there is concordance rates of 5% among dizygotic and 15-30% among monozygotic twins in rheumatoid arthritis. Other than genetic factor, rheumatoid arthritis have been linked with infectious agents (Escherichia coli, proteus species, Epstein - Barr virus and cyto-megalovirus) and their products (heat–shock protein), while some authors suggested molecular mimicry as its cause [2]. Radiographic findings of TMJ arthritis include erosion, osteophytes, sclerosis, subchondral cyst, flattening and reduced joint space. However, flattening of condyle, reduced joint space and osteophytes have been found to be more often in osteoarthritis while erosion of the condyle is more common in rheumatoid arthritis [4]. Cone beam computed tomography (CBCT) being, less costly with lower dose of radiation and minimal distortion has been the method of choice in diagnosing osseous changes at the TMJ [5].
Presented case reports showing erosion at the centre of the condylar surface resembling bifid condyle. However, bifid mandibular condyle is an unusual entity described as a division of the head of the mandibular condyle. Diagnosis of bifid condyle is mainly depends on radiographic evidence due to its minimal symptomatology. Two main etiologies have been suggested for bifid condyle, traumatic and developmental [6]. This paper is highlighting the differential diagnosis between RA and bifid condyle.
Case Report 1
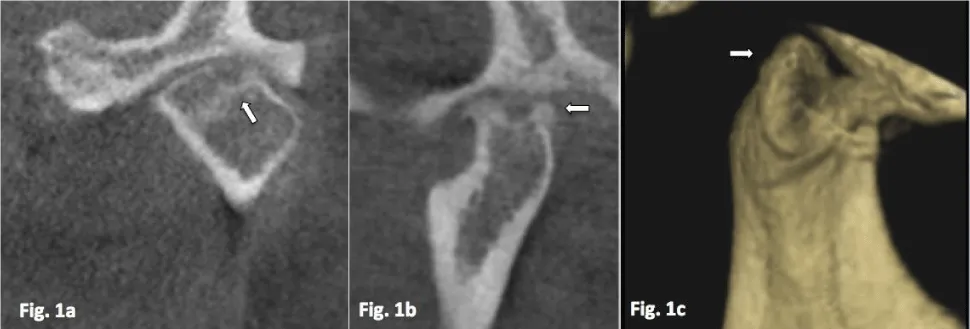
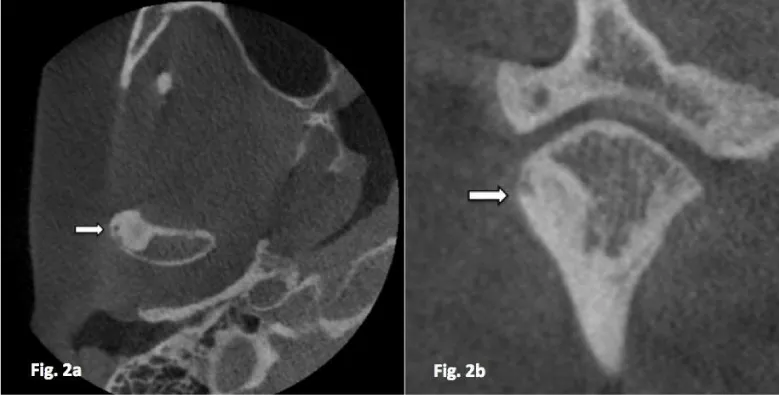
A 56-year-old female patient reported to our department with chief complaint of pain at preauricular region of both sides for three months. Patient was under treatment for RA for four years and was seropositive for rheumatoid factor and anti-citrullinated protein antibodies (>200 RU/ml). Patient gave no history of trauma at TMJ region. On examination, tenderness was present at both TMJ region, and clicking heard at left TMJ while opening the mouth, with restricted mouth opening (36mm). Patient was subjected to CBCT and both TMJ were examined. Coronal view of left TMJ showed erosion by the pannus at the centre of the superior aspect of the left condyle [Figure 1a]. Sagittal and 3D reconstruction views of left TMJ showed marked erosion at the superior aspect of condyle involving half of the condylar head giving appearance of antero-posterior bifid condyle [Figure 1b,c]. This bifid condyle appearance is an unusual radiological finding of TMJ in rheumatoid arthritis. Axial and coronal view of right TMJ revealed marked sclerosis at lateral aspect of condyle, with evidence of subchondral cyst within sclerosed region [Figure 2a,b].
Case Report 2
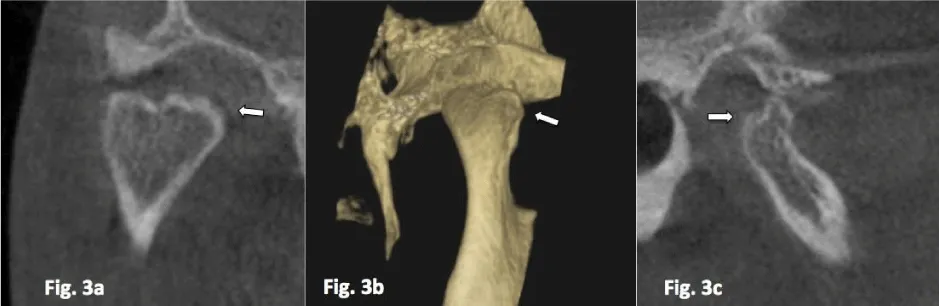
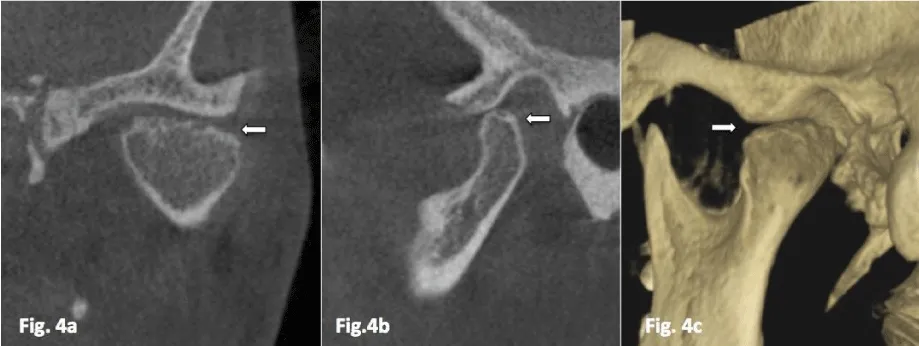
A 62-year-old female reported with chief complaint of pain at left preauricular region for one month. Patient gave no history of trauma at TMJ region and was seropositive for ACPA. (>300 RU/ml) On examination, tenderness was present at left TMJ while opening and closing with normal mouth opening (41mm). For detailed evaluation, CBCT of TMJ was taken. Coronal and 3D reconstructed view of right TMJ showed marked erosion at the centre on superior surface of condyle with loss of continuity of cortical layer giving appearance of mesio distal bifid condyle [Figure 3a,b]. Sagittal view of right TMJ revealed evidence of erosion at the superior surface of the condyle with altered condylar morphology and erosive changes at glenoid fossa was also evident [Figure 3c]. Coronal view of left TMJ revealed erosion on superior surface of the condyle [Figure 4a]. Sagittal view of left TMJ showed evidence of subchondral cyst with well-defined borders on superior surface of condyle [Figure 4b]. 3D reconstruction showed irregular condylar morphology [Figure 4c].
Discussion
Autoimmunity is the main prognostic factor of destructive changes in RA. Autoimmunity and articular erosion is linked by the presence of anti-carbamylated protein antibodies and anti-citrullinated protein antibodies in the serum of RA patients and independently estimate the bony erosion in these patients. When ACPA binds to the cell suface, it causes increase in the osteoclast formation via TNF production [7]. Infection leads to the formation of immune complex which trigger rheumatoid factor production again the Fc region of immunoglobulins which is a known diagnostic marker in rheumatoid arthritis patients [2]. LeResche postulated that pain in the TMJ region is more common in female. It may be explained by influence of prolactin and oestrogen hormones, which causes degenerative changes in particular bone and cartilage by stimulating immunological response at the TMJ [5]. Articular bone erosion involves cortical bone loss and degradation of the natural barrier between the intertrabecular spaces of marrow cavity and the extraskeletal tissues [7]. The synovial pannus produces osteoclast- inducing factors which results in increased resorptive activity at the pannus bone interface [8]. Erosion can be seen as a break in the cortical surface of bone on plain radiographs along with loss of adjacent trabecular bone [7]. There may be erosion of the glenoid fossa and flattening of the articular eminence. As the disease progresses, mandibular condyle shows resorbtive changes [1].
Presented cases showed evidence of arthritic changes in TMJ. In addition to these changes there was evidence of bifidness of the condyles. Factors that lead to bifid condyle are birth injury, trauma, or endocrine disorders [9]. In presented cases none of the factors leading to bifid condyle were present. Moreover, both cases showed evidence of cortical discontinuity because of erosion on the surface of condyle along with other arthritic changes like sclerosis and subchondral cyst. These findings point towards an unexplored dimension that may lead to morphological changes in condyles that can cause appearance of a Pseudo-bifid condyle.
Treatment regimen should be based on the approach to prevent progression of inflammation of the synovial lesion. Studies have shown that the development of bone erosion can be prevented by specifically blocking the activities of TNF [8]. TNF-α blockers were the first approved biologic agents for the treatment of RA [2]. Clinical trials using antirheumatic drugs is also found to retard or arrest the structural damage in RA patients [7]. Bone turnover biomarkers also shows the effectiveness of Anti-inflammatory agents in treating bone loss and suppressing the systemic resorption [2].
Conclusion
Radiologic signs associated with rheumatoid arthritis vary from erosion, osteophytes, sclerosis, subchondral cyst, flattening to reduced joint space. The radiographic findings in these two cases can be confused with the bifid condyle. So, while evaluating the patient presenting with bifid condyle, we should rule out bifidness due to temporomandibular joint arthritis. Correct diagnosis by the clinician should be based on history, clinical, laboratory values and radiographic investigations.
- Bag AK, Gaddikeri S, Singhal A, Hardin S, Tran BD, et al. (2014) Imaging of the temporomandibular joint: An update. World J Radiol 6: 567-582. Link: https://goo.gl/KCPhcp
- McInnes IB, Schett G (2011) The Pathogenesis of Rheumatoid Arthritis. N Engl J Med 365: 2205-2219. Link: https://goo.gl/mX45z9
- Sodhi A, Naik S, Pai A, Anuradha A (2015) Rheumatoid arthritis affecting temporomandibular joint. Contemp Clin Dent 6: 124-127. Link: https://goo.gl/6EJMXB
- Gynther GW, Tronje G (1998) Comparison of arthroscopy and radiography in patients with temporomandibular joint symptoms and generalized arthritis. Dentomaxillofacial Radiology 2: 107–112. Link: https://goo.gl/v79fq8
- Dos Anjos Pontual M, Freire J, Barbosa J, Frazão M, dos Anjos Pontual A, et al. (2012) Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofacial Radiology 41: 24-29. Link: https://goo.gl/HSrfxN
- Jordana X, García C, Palacios M, Chimenos E, Malgosa A (2004) Bifid mandibular condyle: archaeological case report of a rare anomaly. Dentomaxillofac Radiol 33: 278-281. Link: https://goo.gl/mDpYKd
- Schett G, Gravallese E (2012) Bone erosion in rheumatoid arthritis: mechanisms, diagnosis and treatment. Nat Rev Rheumatol 8: 656–664. Link: https://goo.gl/TkJLRO
- Goldring SR (2009) Periarticular bone changes in rheumatoid arthritis: pathophysiological implications and clinical utility. Ann Rheum Dis 68: 1080. Link: https://goo.gl/zf7TE1
- Balaji SM (2010) Bifid mandibular condyle: a study of the clinical features, patterns and morphological variations using CT scans. J Maxillofac Oral Surg 9: 38-41. Link: https://goo.gl/i5r0P4
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
