Annals of Antivirals and Antiretrovirals
Autoimmune hepatitis associated Hepatitis C virus infection treated with first generation direct-acting antivirals
Juan Diego Castro Limo1, Tomás Artaza Varasa1*, María Recuero Pradillo2, Marta Romero-Gutiérrez1, Ana Zaida Gómez Moreno1, Juan José Sánchez Ruano1, Carlos San Román Gutiérrez1, Pablo Muñoz Gómez1 and Rafael Gómez Rodríguez1
2Department of Pathology, Complejo Hospitalario de Toledo, Spain
Cite this as
Castro Limo JD, Varasa TA, Pradillo MR, Gutiérrez MR, Gómez Moreno AZ, et al. (2019) Autoimmune hepatitis associated Hepatitis C virus infection treated with first generation direct-acting antivirals. Ann Antivir Antiretrovir 3(1): 006-008. DOI: 10.17352/aaa.000006Introduction
The hepatitis C virus (HCV) infection has been associated with autoimmune diseases, probably due to the interaction between HCV E2 envelope protein and CD-81 receptor of B lymphocyte and thus, can influence the pathogenesis of autoimmune liver diseases [1,2]. Therefore, it seems reasonable to consider the beneficial effect of direct-acting antivirals (DAAs) for HCV in patients with chronic HCV infection and autoimmune hepatitis (HAI), although evidence is scarce. We report the case of an HCV-infected patient who developed an HAI triggered by interferon and since then has been treated with DAAs improving liver function and maintaining sustained virologic response (SVR), without immunosuppressive treatment nowadays.
Clinical Case
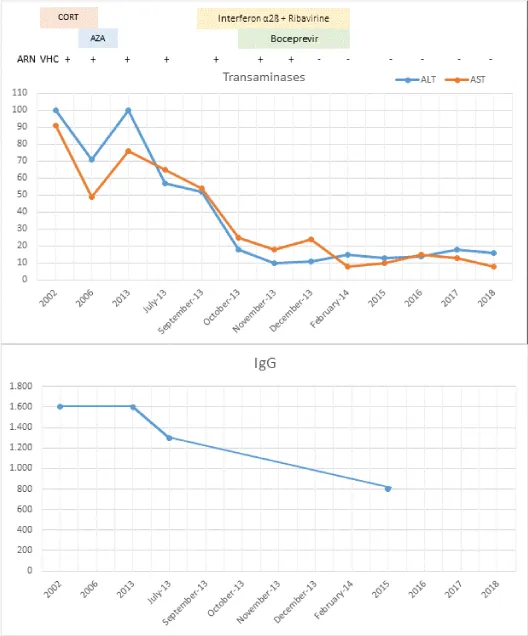
A 54-year-old female was referred to our department in 1995 for elevated aminotransferases, being diagnosed with chronic HCV infection (genotype 1b), with negative metabolic markers, autoimmunity and rest of viral serologies. A liver biopsy was compatible with chronic active hepatitis (Figure 1). For this reason, treatment with interferon alfa-2b was started at 3 MU every 48 hours, but only for two months, due to elevated aminotransferases levels and appearance of high titer anti-LKM type 1 antibodies (1/1280) as well as anti-smooth muscle antibodies (1/40). She was diagnosed with HAI type 2. However, serum IgG values were only slightly elevated. In 2002, immunosuppressive treatment was started with 40 mg prednisone and 100 mg azathioprine, maintained elevated transaminases (Figure 2). In 2003, a new liver biopsy revealed necroinflammatory activity in lobules and stage 2 fibrosis (Figure 2). In September 2013, as the viral load was still positive, we decided to start treatment with Peginterferon alfa-2b (80mcg/week) and Ribavirin (800mg/day) with improvement in transaminases and viral load. For this reason, at 4 weeks of treatment, Boceprevir was added achieving sustained virologic response (SVR). As drug side effects, she presented mild paresthesias, dysgeusia, pruritus, and anemia, which was controlled by decreasing the ribavirin dose. Viral load remained undetectable and antibodies negativized. At this time, we decided to stop immunosuppressive therapy. During the follow-up, she presented cirrhosis in abdominal ultrasound, no varices, and any decompensation episode. Five years after antiviral therapy, she remains asymptomatic, with normal transaminases and SVR (Figure 2).
Discussion
HAI has unknown pathogenesis, however, there seems to be present autoimmune and environmental mechanisms, such as drug use or viral infections; including HCV infection. We report a patient with chronic HCV infection and HAI who improved liver function with DAAs, which reinforces the hypothesis of the HCV involvement in the liver autoimmunity.
The relationship between HAI and HCV can coexist in different clinical situations. In patients with HCV infection, it describes autoantibodies with a probably pathogenic role, for instance, anti-LKM [2,3]. Likewise, HCV can act as an autoimmunity trigger in hepatic and extrahepatic levels, perpetuating damage in the target organ [4]. Finally, there are patients with a rare association called HCV-HAI overlap syndrome who can benefit from antiviral therapy [5]. In addition, it has been described that both interferon and DDAs could be acting as HAI triggers [6,7].
In our case, the patient initially presented chronic liver disease due to HCV infection that was treated with interferon, developing HAI that did not improve with immunosuppressive treatment. For that reason, we started first-generation DDAs, achieving RVS and normal transaminases, so immunosuppressive therapy could be stopped.
On the other hand, few elevated IgG values have been described in HAI patients and positive anti-LKM1, even at the time of diagnosis. As can be seen in figure 1, our patient barely exceeded IgG normal value. She developed cirrhosis over the years, not being present at diagnosis as is also described more frequently in this type of HAI [8].
We found only 3 similar reported cases. First [9], a patient with HAI triggered by interferon and treated subsequently with ledipasvir/sofosbuvir for 12 weeks and with one-year follow-up. The other 2 cases correspond to patients with HAI-HCV overlap syndrome [4,10]. In both, DDAs was effective, improving liver function parameters, but only one of them suspended immunosuppressive therapy with shorter follow-up time. We described the patient with longer follow-up time (5 years) and during this time she has been without immunosuppressive treatment. Moreover, is the only case where first-generation DDAs were used.
Our clinical case seems to confirm the hypothesis suggested by other authors about the determinant role of HCV as a trigger agent of liver autoimmune damage.
Finally, it seems reasonable to confirm in subsequent studies with a large number of patients, if the eradication of HCV would allow permanent suspension of immunosuppressive treatment in selected patients and confirm the treatment as definitely.
- Czaja AJ (2018) Under-evaluated or unassessed pathogenic pathways in autoimmune hepatitis and implications for future management. Dig Dis Sci 63: 1706-1725. Link: https://bit.ly/2nhRbHG
- Shahini E, Iannone A, Romagno D, Armandi A Carparell S, et al. (2018) Clinical relevance of serum non‐organ‐specific antibodies in patients with HCV infection receiving direct‐acting antiviral therapy. Aliment Pharmacol Ther 48: 1138-1145. Link: https://bit.ly/2o95jDs
- Efe C, Heurgue-Berlot A, Ozaslan E, Purnak T, Thiéfin G, et al. (2013) Late autoimmune hepatitis after hepatitis C therapy. Eur J Gastroenterol Hepatol 25: 1308-11. Link: https://bit.ly/2pFBPxq
- Kessel A, Toubi E (2007) Chronic HCV-Related Autoimmunity: A Consequence of Viral Persistence and Lymphotropism. Current Medicinal Chemistry 14: 547. Link: https://bit.ly/2oNUJl4
- Sugiura A, Wada S, Mori H, Kimura T, Matsuda Y, et al. (2017) Successful treatment for chronic hepatitis C-autoimmune hepatitis overlap syndrome due to daclatasvir and asunaprevir. Case Rep Gastroenterol 11: 305-311. Link: https://bit.ly/2oNUVki
- García-Buey L, García-Monzón C, Rodríguez S, Borque MJ, Sánchez AG, et al. (1995) Latent autoimmune hepatitis triggered during interferon therapy in patients with chronic hepatitis C. Gastroenterology 108: 1770-1777. Link: http://bit.ly/2LMxvVu
- Matsumoto K, Kikuchi K, Kajiyama Y, Takano Y, Mabuchi M, et al. (2018) Development of autoimmune hepatitis during direct-acting antiviral therapy for chronic hepatitis C virus infection: a case report. Intern Med 57: 2669-2673. Link: https://bit.ly/2pDw9E1
- Trivedi P, Hubscher S, Heneghan, Gleeson D, Gideon M, et al. (2019) Grand Round: autoimmune hepatitis. J Hepatol 70: 773-784. Link: https://bit.ly/2oS1wKz
- López L, Gómez E, Muñoz R, Tortajada GC, de Andrés CI, et al. (2019) Curación de la hepatitis autoinmune asociada a hepatitis C con antivirales de acción directa. Rev EspEnferm Dig 111: 159-161. Link: https://bit.ly/2nZgoae
- De Maria C, Ghidotti I, Grillo F, Giannini EG (2019) Successful DAA Treatment and Global Improvement in a Cirrhotic Patient with Concomitant HCV Infection and Autoimmune Hepatitis. Dig Dis Sci 64: 591-593. Link: https://bit.ly/2nWDLBf .
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
